CMS Interoperability Framework [Q1 2026 Strategy Guide for Healthcare Leaders]
In July 2025, federal health officials launched the Digital Health Ecosystem initiative featuring a new CMS Interoperability Framework that fundamentally changes how healthcare organizations must approach data sharing.
With concrete federal regulations driving interoperability upgrades on fixed timelines through 2026, CTOs, CIOs, and Chief Strategy Officers can no longer treat interoperability as a future consideration. The Q1 2026 deadline for CMS Aligned Networks isn't negotiable, and organizations that miss compliance face severe financial penalties and competitive disadvantages.
For PE-backed specialty clinics consolidating disparate EHRs into unified platforms, this regulatory environment creates both urgent compliance requirements and strategic opportunities. Success requires immediate action, comprehensive planning, and expert implementation support.
This analysis draws insights from leading industry voices, including Brendan Keller, author of the Health API Guy newsletter. His expertise on healthcare interoperability infrastructure provides critical context for understanding the strategic implications of these regulatory shifts.
The New Interoperability Imperative
The July 2025 CMS Health Tech Ecosystem Initiative secured pledges from over 60 major healthcare organizations to collaborate on a "next-generation" patient-centric healthcare experience. This isn't just another voluntary framework – it represents industry-wide momentum that will define competitive positioning for the next decade.
Twenty-one national health networks have already committed to meet the CMS Interoperability Framework criteria, becoming "CMS Aligned Networks." Leading health systems and EHR vendors have agreed to support comprehensive patient data access and even "kill the clipboard" by replacing paper intake forms with digital workflows.
The implications extend far beyond compliance. 67% of CIOs cite interoperability as their biggest digital transformation barrier, yet the new framework makes delay impossible. Organizations that achieve early compliance gain significant competitive advantages in patient acquisition, payer relationships, and care quality metrics.
For PE portfolio companies, the stakes are particularly high. Exit valuations increasingly depend on technological sophistication and operational efficiency – both directly tied to interoperability capabilities.
Breaking Down the CMS Interoperability Framework
What CMS Aligned Networks Actually Means
CMS Aligned Networks represent a fundamental shift from data availability to active participation in interconnected healthcare ecosystems. The framework establishes ambitious data-sharing principles that go beyond traditional HIE connections.
Key objectives include enabling patients to access all electronic health information through apps of their choice, allowing providers to query and retrieve records for treatment with minimal friction, and ensuring standardized data formats and APIs across networks.
By July 4, 2026, networks must expose data via modern FHIR APIs aligned with the US Core Implementation Guide and USCDI v3. This means underlying EHR systems must share patient records in real time using the HL7 FHIR standard, including structured data like labs (LOINC), medications (RxNorm), and conditions (SNOMED CT).
The framework also emphasizes secure digital identity standards. Patients shouldn't need multiple logins; instead, a CMS-approved digital ID should be universally honored across aligned networks.
How This Differs From Previous TEFCA Framework
While TEFCA focused on establishing basic connectivity between health information networks, CMS Aligned Networks demand active intelligence sharing and collaborative care coordination. TEFCA went live in early 2023 as a "network of networks," but the new CMS framework requires deeper integration and real-time data processing capabilities.
CMS has indicated it will join these networks itself – by Q1 2026, Medicare's Blue Button 2.0 claims data will be queryable through the framework. This government participation signals the framework's importance and permanence.
The choice by CMS was to set the bar well beyond where TEFCA or any network currently operates, creating competition between networks to rise to the occasion rather than attempting to influence existing collaborative frameworks from a subordinate position.
Why This Matters for Healthcare Leaders Now
Executive Demands and PE Expectations
Board meetings at healthcare organizations now include interoperability as a standard agenda item. Directors want concrete answers about compliance timelines, implementation costs, and competitive implications. The regulatory landscape has shifted from voluntary adoption to mandatory participation.
PE investors add another layer of urgency. Portfolio companies must demonstrate technological sophistication to attract premium exit valuations. Interoperability capabilities directly impact operational efficiency metrics that drive investment returns.
The pressure extends beyond avoiding penalties. Organizations that establish strong positions within CMS Aligned Networks benefit from increasing data quality, expanded partnership opportunities, and enhanced competitive differentiation.
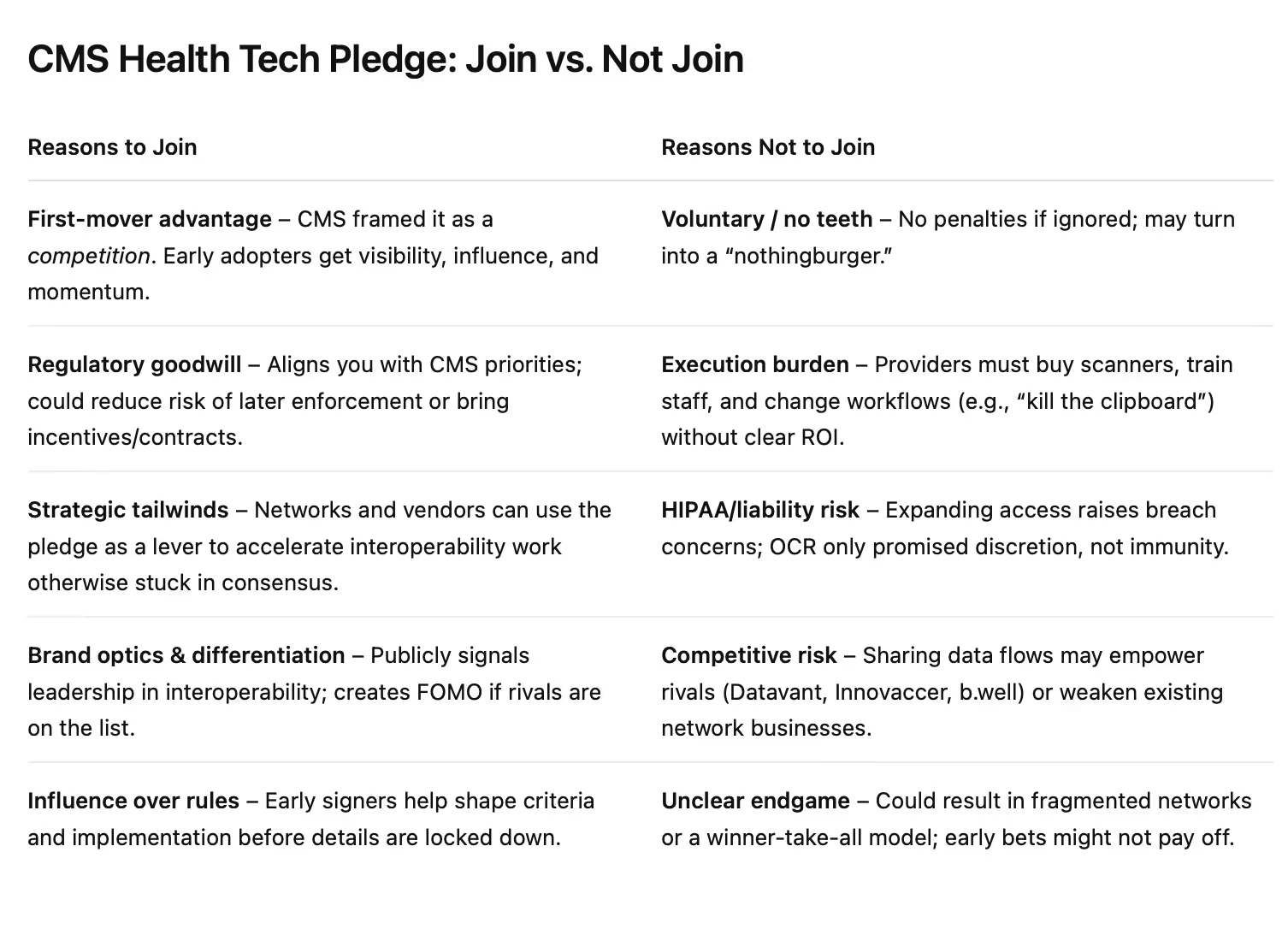
Understanding the Pledge Strategy Behind the Framework
The CMS deliberately chose a pledge format over traditional rulemaking for strategic reasons that healthcare executives must understand. Speed was the primary driver – traditional regulatory processes would have taken years to crystallize, with implementation deadlines extending into 2027 or 2028.
This voluntary collaboration creates powerful motivators without regulatory overhead. The framework essentially pits networks against one another in a race to achieve CMS Aligned Network status and reap the benefits of government participation and favor. The competitive aspect has already generated significant interest, with organizations actively seeking ways to participate.
Moreover, this administration operates in a supposed deregulatory environment, making voluntary pledges politically palatable while achieving the same policy goals as mandates. The CMS retains the option to add incentives, penalties, or additional requirements as the initiative evolves.
Key Regulatory Requirements Through 2026
21st Century Cures Act & ONC Certification Timeline
The regulatory foundation rests on concrete federal mandates with non-negotiable deadlines. The 21st Century Cures Act and ONC certification requirements established new standards for certified EHR technology, with "Cures Act Edition" updates required by 2022.
The bar is rising again. ONC's latest Health Data, Technology, and Interoperability (HTI-1) final rule has adopted United States Core Data for Interoperability version 3 (USCDI v3) as the new baseline. Certified health IT must accommodate USCDI v3 data using FHIR US Core profiles by January 1, 2026.
This means a EHR vendor should be rolling out updates by 2025 to include richer data elements such as social determinants of health, health insurance information, and other additions in USCDI v3. When evaluating EHR solutions, verify that the product is ONC-certified and on track for the 2025/2026 certification updates.
Information Blocking Rule & Severe Penalties
The 21st Century Cures Act prohibits "information blocking" by healthcare providers – any practice likely to interfere with the access, exchange, or use of electronic health information. Since April 2021, providers have been required to make core clinical data (USCDI) accessible by default.
Enforcement has intensified dramatically. As of July 2024, healthcare providers face severe disincentives if found engaging in information blocking. A hospital that unreasonably impedes data sharing could lose 75% of its Medicare annual payment update. A physician practice could receive a zero score in the Promoting Interoperability category of MIPS, directly hurting reimbursement.
These penalties can significantly impact revenue. CTOs must ensure their organizations have policies and technologies in place to share data appropriately, including enabling patients to download or transmit their full records and responding promptly to record requests from other providers.
CMS Interoperability & Patient Access Requirements
The CMS Interoperability and Patient Access final rule required Medicare Advantage and Medicaid plans to launch patient-facing APIs by 2021. The Advancing Interoperability and Improving Prior Authorization Rule adds significant requirements.
By 2026, payers including Medicare Advantage, Medicaid, and ACA exchange plans must implement FHIR-based APIs for patient access and exchanging data with providers, including prior authorization status. Starting in 2027, physicians will have a new measure in MIPS for using Electronic Prior Authorization technology.
Specialty clinics should prepare to integrate with these new payer APIs, replacing today's inefficient fax and portal processes with digital prior authorization workflows within EHR systems.
Understanding TEFCA and CMS Framework Alignment
TEFCA provides a nationwide trust framework for health information exchange through Qualified Health Information Networks (QHINs). While not mandatory, TEFCA offers a single on-ramp to exchange data with a broad range of participants nationwide.
The CMS framework aligns conceptually with TEFCA, and CMS plans to use CMS-Aligned Networks for its own data sharing. If your current EHR vendor or HIE partner participates in TEFCA, it could greatly expand your reach in obtaining outside records for comprehensive patient care.
Technical Architecture Requirements for Compliance
FHIR-Based API Implementation Standards
The foundation of CMS compliance rests on FHIR R4 API implementation, but technical success requires more than basic standards compliance. The architecture must support high-volume, real-time data exchanges while maintaining sub-second response times.
Modern API management platforms become essential infrastructure components. Rate limiting, authentication, monitoring, and version control capabilities aren't optional – they're regulatory requirements. A technical team needs to architect for scale from day one.
Ensure support for OAuth 2.0/OpenID Connect standards for API security, as these are used by third-party apps that patients or partners might use to connect to EHR data.
Integration complexity varies significantly based on existing:
- EHR infrastructure
- Organizations using Epic
- Oracle Health
- Other major platforms with built-in advantages
Security, Privacy, and Identity Management
HIPAA compliance takes on new dimensions within CMS Aligned Networks. The framework explicitly calls for networks to support strong digital credentials (NIST Identity Assurance Level 2) for patients and providers, and to maintain high security certifications like HITRUST.
Identity and access management systems need complete overhauls in many organizations. Single sign-on capabilities, multi-factor authentication, and role-based access controls must work seamlessly across network participants.
Data encryption requirements extend beyond storage to include all transmission channels. End-to-end encryption becomes a baseline requirement rather than an advanced security feature. Robust audit logging is essential – you need to track who accessed what information for compliance and to build patient trust.
Strategic Implementation Roadmap to Q1 2026
Reframing Interoperability as Ongoing Infrastructure
Before diving into implementation phases, healthcare executives must fundamentally reframe their understanding of interoperability. "Interoperability is infrastructure - imagining it as a solvable checkbox problem rather than a series of ongoing investments towards new functionalities and features is your problem," observes Brendan Keller.
This perspective is crucial for proper resource allocation and expectations management. The Q1 2026 deadline isn't the finish line – it's the starting point for continuous infrastructure investment. Just as no organization considers roads or privacy "solved," interoperability requires ongoing attention, updates, and enhancement.
The arc of progress when building infrastructure across tens of thousands of organizations means that the change of a decade is taken for granted, while the change of a year is nearly invisible. Two decades ago, every prescription was printed on paper. That interoperability problem was solved with regulatory nudges and market consolidation. A decade ago, providers didn't have access to longitudinal records from other providers – that's significantly closer to being solved today through existing networks.
Three-Phase Implementation Approach
Phase 1
Phase 1 (Q3 2025) focuses on comprehensive assessment and gap analysis. The technical team needs to evaluate current infrastructure capabilities against CMS requirements, including API readiness, security frameworks, and data governance policies.
Don't underestimate assessment complexity. Many organizations discover that their "FHIR-ready" systems need significant upgrades to meet real-world interoperability demands. Budget extra time for thorough testing and validation.
Phase 2
Phase 2 (Q4 2025) centers on vendor selection and architectural planning. The vendor landscape evolves rapidly, with new solutions emerging monthly. Evaluation criteria must balance technical capabilities with implementation timelines and ongoing support requirements.
Phase 3
Phase 3 (Q1 2026) involves full implementation and testing. However, testing isn't just technical validation – it requires real-world data exchanges with network participants. Plan for multiple integration cycles and extensive user acceptance testing.
Risk mitigation strategies are crucial for each phase. Technical risks include integration failures and performance bottlenecks. Business risks involve compliance delays and competitive disadvantages. Financial risks encompass budget overruns and unexpected resource requirements.
Evaluating EHR Solutions for Interoperability
Certification and Standards Requirements
When evaluating EHR solutions for interoperability compliance, certification verification is non-negotiable. Ensure any EHR under consideration is ONC-certified to the latest standards, including the 2015 Edition Cures Update and readiness for HTI-1 2025 requirements.
Ask vendors about their roadmap for supporting USCDI v3 and FHIR API enhancements by 2026. You want concrete assurances that the system will keep you compliant with federal rules. An EHR that natively supports FHIR endpoints for patient data, bulk data export, and standardized code sets (LOINC, SNOMED, etc.) will reduce custom development needs.
Exchange and Integration Features
Analyze the EHR's ability to interoperate with external systems. Key features include connectivity to health information exchanges or networks (CommonWell, Carequality, or local HIE out of the box), support for Direct Messaging or other referral exchange methods, and built-in API endpoints to communicate with specialty systems, labs, and payers.
If consolidating multiple sites, you'll need data migration capabilities. Check if the vendor provides tools for data import/export in standardized formats like CCDA documents or bulk FHIR import to port patient records from legacy systems.
Consider interoperability middleware or interface engines during transitions. Some organizations deploy unified data layers that aggregate data from multiple EHRs into common repositories, useful during phased rollouts while maintaining comprehensive patient records.
ROI Calculations and Budget Planning
Real Implementation Costs and Hidden Expenses
Mid-market healthcare organizations typically invest between $500,000 and $2.5 million in comprehensive interoperability implementations. However, these figures only represent direct technology costs. Hidden expenses often double the total investment.
Staff training represents a significant but often underestimated expense. Clinical and administrative teams need extensive education on new workflows and system capabilities. Plan for 40-60 hours of training per user across multiple sessions.
Ongoing maintenance and support costs continue indefinitely. API management, security monitoring, and system updates require dedicated resources. Budget for at least 20% of initial implementation costs annually for ongoing operations.
PE exit valuations increasingly reflect technological sophistication and operational efficiency. Organizations with advanced interoperability capabilities command premium multiples due to reduced operational risks and improved growth potential.
Strategic Benefits of Early Adoption
Early compliance with CMS Aligned Networks creates multiple competitive advantages beyond regulatory requirements. Patient acquisition becomes easier when an organization can provide seamless care coordination and comprehensive health records access.
Payer relationships improve dramatically when administrative processes integrate smoothly with insurance systems. Prior authorization delays decrease, claims processing accelerates, and patient satisfaction scores increase.
Partnership opportunities emerge naturally within CMS Aligned Networks. Healthcare organizations that demonstrate technical sophistication and operational excellence become preferred partners for referrals and collaborative care agreements.
Clinical outcomes improve when providers have real-time access to comprehensive patient histories. Care coordination reduces duplicative testing, prevents medication conflicts, and enables proactive intervention strategies.
The Race for CMS Aligned Network Status
The competitive dynamics of the pledge system create powerful incentives for early adoption. The CMS is essentially pitting networks against one another in a race to achieve aligned network status and reap the benefits of government participation and favor.
This competitive element has already generated significant FOMO (fear of missing out) effects across the industry. Organizations that achieve early compliance gain not just regulatory advantages but also preferential positioning for future government contracts and partnerships.
The network effect becomes particularly powerful over time. Organizations that establish strong positions within CMS Aligned Networks benefit from increasing data quality, expanded partnership opportunities, and enhanced competitive differentiation.
Multi-Site EHR Consolidation Best Practices
For CTOs overseeing transitions from multiple EMRs to unified systems, strategic phased approaches are essential to minimize disruption while meeting regulatory goals.
Develop unified data strategies early. Before new systems go live, normalize data across sites. If different clinics use different coding practices, decide on common coding standards aligned with national standards. This makes migrating data cleaner and facilitates interoperability since standards like LOINC for labs and RxNorm for medications are expected under USCDI.
Leverage interface engines during cutover periods. When not all sites are on new EHRs, use integration platforms to mirror key data between systems. This prevents gaps in patient records and maintains data repository completeness.
Training and change management are crucial. Staff and clinicians must learn new tools and workflows that promote data sharing. Make interoperability a theme in training, highlighting how to query external HIEs, fulfill patient data requests, and document referrals that automatically generate appropriate summaries.
Timeline alignment with regulatory milestones is critical. If the goal is full EHR consolidation by late 2025, that positions you well to meet Q1 2026 interoperability objectives and January 2026 certification changes.
4 Possible Outcomes for the Industry
Brendan Keller had a great take on potential industry outcomes. Based on historical patterns and current market dynamics, the CMS initiative could evolve in four distinct directions, each with different implications for healthcare executives.
Scenario 1
The first scenario involves interconnected, ubiquitous networks. Multiple sub-networks meet CMS criteria but create an interoperable fabric so that from a provider's perspective, it feels like one unified system. Competition exists behind the scenes for pricing and value-added services, but the front-end experience feels universal.
Scenario 2
A second possibility is winner-take-all ubiquity, where one network gains both policy favor and market share, becoming effectively the only viable path. Everyone connects to this dominant network because CMS rules and certification criteria make it unavoidable.
Scenario 3
This scenario produces parallel, competing, fragmented networks. Coverage becomes patchy, with some regions and use cases deeply served while others lack access entirely. Users constantly hit dead ends because their counterparties are "on the other network."
Scenario 4
This option creates parallel, competing, ubiquitous networks. Two or more heavyweight networks each reach near-total coverage but don't merge or fully interconnect. End users might need to support multiple rails, but this creates beneficial competition on price, features, and quality while providing system resilience.
"If your bar of success is 'will we have solved interoperability?', the unfortunate reality is that you'll never be satisfied," notes Brendan. The key is defining realistic success metrics and appropriate time horizons for measuring progress.
Final Takeaways
The CMS Health Tech Ecosystem Initiative represents both regulatory requirements and strategic opportunity for healthcare organizations. Success demands immediate action, comprehensive planning, and expert implementation support.
CTOs, CIOs, and Chief Strategy Officers who approach this challenge strategically will position their organizations for competitive advantage, operational excellence, and premium exit valuations. However, the Q1 2026 deadline demands urgent attention to assessment, planning, and implementation activities.
The regulatory landscape is unforgiving. Information blocking penalties can cost organizations 75% of Medicare payments. USCDI v3 compliance is mandatory by January 1, 2026. Prior authorization requirements reshape payer relationships by 2027.
Yet organizations that invest in comprehensive interoperability strategies gain sustainable competitive advantages. They excel in value-based care contracts, multi-site expansions, and patient loyalty. They attract investors and partners because integrated data demonstrates outcomes and efficiencies.
The federal push ensures that healthcare IT's future is open and connected. This initiative will make progress, prove out technologies, and advance the industry – while simultaneously uncovering new problems to solve and the next generation of infrastructure to build. That's not failure; that's the nature of infrastructure development.
Embracing this reality with clear strategy and robust technology will set your organization apart as a leader in coordinated care delivery.
Frequently Asked Questions
What are the specific penalties for missing the January 1, 2026 USCDI v3 compliance deadline?
Non-compliant organizations face exclusion from ONC certification requirements, which can impact Medicare reimbursement and market competitiveness. More immediately, information blocking violations can result in hospitals losing 75% of Medicare annual payment updates and physician practices receiving zero scores in MIPS Promoting Interoperability categories.
How do CMS Aligned Networks differ from current TEFCA participation?
CMS Aligned Networks require active participation and bi-directional real-time data sharing, while TEFCA often relies on query-based access. The new framework demands collaborative care coordination and integration with Medicare's Blue Button 2.0 data by Q1 2026, going beyond TEFCA's network connectivity approach. The CMS set the bar well beyond where TEFCA currently operates, essentially daring existing networks to keep up.
What's the typical implementation timeline for organizations consolidating multiple EHR systems?
Most organizations require 6-9 months for comprehensive implementation, but multi-site consolidation can extend to 12-18 months depending on complexity. Given the Q1 2026 deadline, organizations should begin assessment phases immediately in Q3 2025 to ensure compliance readiness.
Can organizations use multiple vendors for different aspects of CMS Framework compliance?
Yes, hybrid approaches are common and often recommended. Many organizations combine EHR vendor solutions with specialized integration platforms like those offered by companies with deep healthcare software development expertise, optimizing costs and capabilities while meeting comprehensive compliance requirements.
What ongoing technical resources are required to maintain CMS Aligned Network compliance?
Plan for dedicated technical staff equivalent to 1-2 FTE positions, plus ongoing vendor support and system maintenance costs. Organizations also require periodic consulting support for API management, security monitoring, system updates, and regulatory compliance tracking as requirements evolve through 2027 and beyond. Remember that interoperability is ongoing infrastructure investment, not a one-time project.
James founded Invene with a 20-year plan to build the world's leasing partner for healthcare innovation. A Forbes Next 1000 honoree, James specializes in helping mid-market and enterprise healthcare companies build AI-driven solutions with measurable PnL impact. Under his leadership, Invene has worked with 20 of the Fortune 100, achieved 22 FDA clearances, and launched over 400 products for their clients. James is known for driving results at the intersection of technology, healthcare, and business.
Ready to Tackle Your Hardest Data and Product Challenges?
We can accelerate your goals and drive measurable results.

