Medicare Advantage Star Ratings: Fast, Cost-Effective Improvement Strategies for COOs

Medicare Advantage star ratings just dropped, and the board meeting is next week. Sound familiar? Thousands of COOs across the country are staring at disappointing CMS star ratings wondering how to turn things around without breaking the bank.
Here's what most executives miss: the best star rating improvements deliver immediate business value like cost savings and operational efficiency. While your competitors scramble for expensive, long-term infrastructure overhauls, smart COOs are finding initiatives that kill two birds with one stone.
This is about working smarter, not harder. Let's dive into the strategies that successful regional and PE-backed plans use to quickly boost their ratings while delivering other measurable business outcomes.
The Real Economics of Star Rating Improvements (And Why 5 Stars Isn't Always Better)
Before you start chasing that perfect five-star rating, let's talk economics. Many COOs don't realize that the math behind star ratings is more complex than it appears on the surface.
The 4.5 Star Sweet Spot
For most Medicare Advantage plans, 4.5 stars is often the optimal target rather than the maximum five-star rating. This is about understanding the economic realities of Medicare Advantage enrollment patterns.
At 4.5 stars, you still receive quality bonus payments from CMS without triggering the enrollment challenges that come with five-star status. You get the financial benefits of higher ratings while maintaining better control over your risk pool composition.
Think of it like driving a car. You could push the pedal to the floor and hit maximum speed, but you'd burn through fuel and risk mechanical problems. The sweet spot is finding the speed that gets you where you need to go efficiently and safely.
The Reality of 5-Star Status
Five-star plans unlock year-round enrollment and marketing advantages that appear beneficial on paper. However, a financial reality exists behind those benefits that many regional payers don't fully understand until implementation.
These plans attract members with higher care needs who actively use the enhanced benefits these plans are required to offer. Members managing multiple chronic conditions gravitate toward plans with the most comprehensive coverage and lowest out-of-pocket costs.
Members are enrolled and engaged. They use wellness visits, fill prescriptions, and access preventive care that drives up medical loss ratios.
CMS expects this outcome. The risk adjustment model accounts for higher-cost populations through HCC coding, but the financial mechanics still require careful planning. Plans operate with higher per-member costs while delivering the enhanced benefits that earned the five-star rating.
The challenge isn't system unfairness. Many plans chase five-star status without building the operational infrastructure to manage increased utilization. Care management programs require greater sophistication, provider networks need more robust capacity, and financial projections demand more nuanced modeling.
For most regional plans, targeting 4.5 stars delivers quality bonus payments without requiring the same level of enhanced benefits and operational complexity. Plans receive meaningful CMS bonuses while maintaining more predictable utilization patterns that align with actuarial models and network capacity.
Data Access: The Hidden Advantage That Changes Everything
Most Medicare Advantage plans are fighting star rating battles with one hand tied behind their back. They're stuck analyzing only claims data. It’s more advantageous to have access to both claims and clinical data because your ability to do population analytics improves drastically.
Claims vs Clinical Data: Understanding the Advantage
Claims data tells organizations what happened after the fact. A member had a hospital admission, received a prescription, or visited a specialist. It's historical and reactive. Clinical data tells organizations what's happening right now and what might happen next. Lab values, vital signs, care plans, and provider notes give a real-time picture of member health status.
It's not uncommon for members to drop out of treatment and for plans to lose data on them. The technical term for this is called data "censoring." For example, if someone is referred for a mammogram and there are no further claims after that, then what happened? Did they find nothing? Did they move out of network because they got aggressive cancer? Did they die? Not to be morbid, but it's a real issue in the data.
A major benefit of EHR data lies in its comprehensive clinical context. Claims data captures only billing codes and procedure information. EHRs contain detailed clinical narratives, precise quantitative measurements, diagnostic images, and thorough documentation from each patient encounter. This depth enables organizations to better understand how diseases present and progress, why specific treatments were chosen and how patients responded, and the overall complexity of individual cases.
EHR systems also aggregate patient records across extensive healthcare networks, creating real-world datasets encompassing millions of patient interactions. This scale provides insights into treatment patterns and outcomes that claims data simply cannot deliver.
When both datasets are combined, organizations unlock population analytics capabilities that can dramatically improve star ratings. Plans can identify gaps in care before they become expensive problems. Organizations can predict which members are at risk for complications and intervene proactively.
While data integration can be difficult, data access is the real challenge. If data already lives in an OLAP data lake like ClickHouse or Snowflake, organizations can begin analytics work immediately. The problem is getting it there in the first place.
Predictive Analytics: Your Own Data Beats Off-the-Shelf Every Time
In predictive analytics, use cases fall into two distinct categories that require completely different approaches:
- OPD (Other People's Data)
- YODA (Your Own Data Analytics)
With OPD you can use off the shelf models and data to derive useful insights. It works great for macro trends. Think economic modeling or population health patterns at the federal level. These are situations where larger datasets provide better insights because you're looking for broad patterns that apply across diverse populations.
But when it comes to Medicare Advantage star ratings, you're dealing with YODA territory. The nuances of your specific member population get averaged out when you use larger macro-trend data. Your members in rural Oklahoma have different health patterns, provider relationships, and care-seeking behaviors than members in urban California.
With predictive analytics for Stars, the holy grail is outreach at the individual member level. That means knowing exactly which members need attention and when. To get there, you need a deep understanding of your population, and this is where AI/ML adds real value. Instead of generic risk flags, custom models can pinpoint which of your members are at risk, enabling targeted interventions that move your quality scores.
This is actually where regional plans with around 3,000 members have a huge advantage. Your population is small enough to analyze at the individual member level, but large enough to identify meaningful patterns. You can spot risks and opportunities that get lost in the noise of larger datasets.
The bottom line for Medicare Advantage organizations: real value comes from building custom predictive models and analyzing member data at the individual level. Off-the-shelf solutions won't capture the specific nuances that drive your star rating performance.
The best applications are the ones you build yourself, tailored to your specific member demographics and care patterns. Off-the-shelf solutions might give you insights about Medicare Advantage members in general, but they won't tell you about YOUR Medicare Advantage members specifically.
This same principle applies to patient experience monitoring. Advanced patient experience platforms use real-time data to prevent quality gaps before they impact CAHPS scores, rather than waiting for quarterly survey results to identify problems.
Double-Dip Strategies: Quality Improvements That Also Save Money
Quality initiatives struggle to get funded because they're viewed as long-term investments with unclear ROI. The solution is identifying initiatives that improve star ratings while delivering immediate business value like cost avoidance.
Population-First Resource Allocation
Most executives start by analyzing individual HEDIS measures, but this approach misses the bigger picture. Start with population and member-level analysis first, then determine which quality domains and specific measures matter most for the plan's unique membership.
Member and provider outreach represent the primary levers for affecting star rating changes. Predictive analytics and population data analysis exist to answer three critical resource allocation questions:
- Where should limited resources be invested?
- Which members should receive outreach first?
- What specific health issues cause the most problems for the member population?
Quality Domain Impact Analysis
Different quality domains offer varying returns on investment based on member demographics and health status. Care coordination measures typically provide high impact for older populations with multiple chronic conditions. Medication adherence measures often deliver strong ROI across age groups while reducing pharmacy costs.
Preventive care measures like cancer screenings may offer limited short-term returns for younger populations but can be valuable for plans serving older demographics. The key is matching quality domain focus to actual member needs rather than trying to improve all measures equally.
Short-Term ROI Paired with Quality Improvements
Since quality improvement is difficult to fund as a standalone initiative, successful programs pair immediate cost savings with star rating improvements. Care management programs that reduce emergency department utilization show measurable cost reductions within months while improving care coordination scores.
Provider engagement initiatives that reduce duplicate testing and improve referral efficiency deliver operational cost savings alongside better care coordination measures. Medication therapy management programs can reduce drug costs through generic substitutions while improving adherence scores.
The dual-value approach makes quality initiatives competitive with other budget priorities during planning cycles. When quality improvements also drive cost reduction, finance teams can justify the investment based on immediate returns rather than waiting for long-term quality outcomes.
Organizational Reality Check: Why Most Star Rating Initiatives Fail
Most star rating initiatives fail not because of poor strategy, but because of organizational misalignment. Different departments look at the same data and reach different conclusions.
Data Alignment Challenges
Quality teams focus on clinical outcomes while finance teams worry about costs. Operations teams care about workflow efficiency. When departments use different data definitions, member attribution rules, and measurement timeframes, they generate conflicting performance reports from identical source data.
These different perspectives lead to conflicting priorities and resource allocation decisions. Data structure creates different analytical conclusions from the same information, which undermines initiative effectiveness.
Organizational alignment on data ingestion and analysis methodology matters more than technology platforms. Advanced analytics capabilities cannot overcome fundamental disagreements about basic definitions and measurements between departments.
Funding Quality Initiatives
Quality initiatives often end up lowest priority when budget allocations get set. They compete against revenue-generating programs and cost-cutting measures that show immediate results. Short-term wins that demonstrate measurable ROI build momentum for longer-term quality investments.
Successful plans create cross-functional teams that include quality, finance, operations, and analytics from day one. They establish common definitions, shared metrics, and aligned incentives before launching initiatives.
When quality improvements also deliver cost savings or operational efficiency gains, they compete more effectively for budget allocation. Finance teams support initiatives that improve the bottom line while enhancing quality outcomes.
Implementation Playbook: Quick Wins in 6 Months
Time is critical when it comes to star rating improvements. You want 6 month quick wins and 18 month transformational changes.
CAHPS surveys go out in March, and those determine next year's ratings. Your quick wins have to come before that deadline, or you're not impacting anything until the following year.
Member Outreach Campaigns
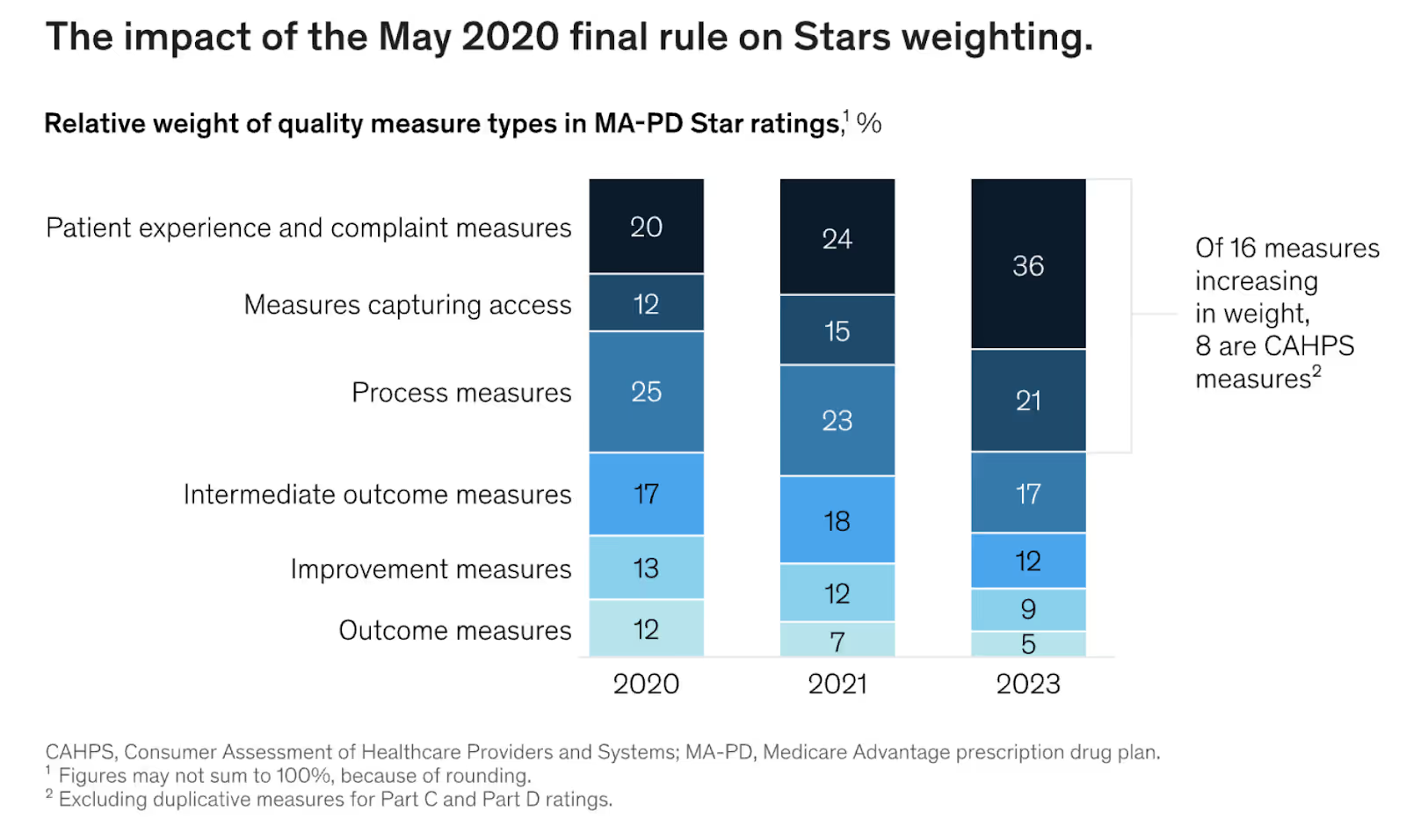
CMS elevated the weight of customer experience to 57% in evaluating MA plan quality. Member outreach campaigns that impact multiple measures simultaneously should be your first priority.
Design programs that address medication adherence, preventive care, and care coordination in one integrated approach. Instead of separate campaigns for each quality measure, create holistic member engagement that touches multiple domains.
For example, a comprehensive diabetes management outreach program can improve HbA1c testing rates, blood pressure screening, cholesterol management, and medication adherence all at once. You're leveraging one campaign to move multiple quality measures while providing real value to members.
Focus on members who are identified through your predictive analytics as having the highest probability of improvement with minimal intervention. These are typically members who are engaged with care but have small gaps that can be easily addressed.
Provider Engagement Programs
Provider engagement strategies that improve care coordination and quality scores work particularly well for quick wins. Most providers want to deliver better care but lack the data and support to do it effectively. Give them actionable insights about their patients and clear pathways for improvement.
Create provider-facing dashboards that show quality measure performance for their patient panels. Include specific patient lists with recommended actions. Make it easy for providers to see which of their diabetic patients need HbA1c tests or which members are overdue for colorectal cancer screening.
Support these insights with care coordination tools that make it easier for providers to close quality gaps. Pre-populate referral forms, automate appointment scheduling for preventive services, and provide decision support tools that integrate with existing workflows.
Data Infrastructure Quick Wins
Data access improvements don't require massive system overhauls if you're strategic. Focus on getting the most critical data streams flowing first. You don't need perfect integration on day one. You need good enough data to start making better decisions and measuring outcomes.
Start with the data you already have and improve its usability. Clean up member demographic information, standardize provider data, and create consistent definitions across departments. These foundational improvements will make your existing analytics more reliable and actionable.
Then add one new data stream at a time. If you have claims data, add pharmacy data next. If you have both, add lab results or provider notes. Each additional data source multiplies the value of your existing information without requiring a complete technology overhaul.
Measure success by tracking both star rating improvements and business value delivery. Create dashboards that show quality metrics alongside cost savings, member satisfaction scores, and operational efficiency measures. This dual tracking helps sustain executive support and builds the business case for continued investment.
Final Takeaways
Improving Medicare Advantage star ratings doesn't have to break your budget or require years of infrastructure investment. The most successful COOs find initiatives that improve quality scores while delivering immediate business value like cost savings and operational efficiency.
Focus on your own data instead of off-the-shelf solutions. Your member population has unique characteristics that generic models can't capture. Regional plans actually have advantages here because they can analyze at the individual member level.
Start with member and provider outreach as your primary levers for change. Design programs that hit multiple quality domains simultaneously while solving other business problems. This dual-purpose approach makes quality initiatives easier to fund and sustain.
Most importantly, get your organizational alignment right before investing in new technology. The fanciest analytics platform won't help if departments can't agree on basic definitions and measurements.
Remember, ratings come out in October, and that's when plans scramble to find ways to improve. But the smart money starts planning in November for the following year's ratings. While everyone else is reacting, you should be executing a well-planned strategy.
The next open enrollment period is coming whether you're ready or not. The question is: will you be scrambling with everyone else, or will you be executing a strategic plan that delivers both better quality and better business outcomes?
Frequently Asked Questions
What's the fastest way to improve Medicare Advantage star ratings without major technology investments?
Focus on member and provider outreach campaigns that target multiple quality measures simultaneously. These programs can show results within 6 months and typically require minimal technology investment while delivering both quality improvements and cost savings.
Why should regional Medicare Advantage plans avoid trying to reach 5-star status?
Five-star plans face continuous enrollment of high-risk members who disenroll at three times the normal rate. For most regional plans, 4.5 stars provides quality bonus payments without the revolving door of high-cost membership that can destroy your medical loss ratio.
How can Medicare Advantage plans get better data without expensive system overhauls?
Start by improving data access rather than data integration. If you already have claims data, focus on adding clinical data streams to your existing analytics platform. The key is having both datasets available for analysis, not perfect integration on day one.
Which quality domains offer the highest return on investment for star rating improvements?
It depends on your member demographics, but care coordination and medication adherence typically offer the best ROI because they impact multiple measures simultaneously while reducing costs through better outcomes and fewer complications.
How do successful Medicare Advantage plans get quality initiatives funded when budgets are tight?
They design initiatives that deliver immediate business value alongside quality improvements. For example, diabetes management programs that improve screening rates while reducing emergency department visits and hospital readmissions show measurable cost savings within the first year.
Alex leads Invene's engineering teams to deliver secure, compliant, and deadline-driven healthcare solutions. Previously, he successfully exited his own consulting company, where he built innovative products integrating hardware and software. He's passionate about speaking and helping business leaders understand technology so they can make better, more informed decisions. He also mentors engineers and regularly explores white papers to stay ahead of the latest technological advancements.
Ready to Tackle Your Hardest Data and Product Challenges?
We can accelerate your goals and drive measurable results.

