Cerner EHR Strategic Assessment for Post-Oracle Acquisition

Healthcare technology executives face unprecedented complexity when evaluating electronic health record (EHR) solutions today. Oracle's acquisition of Cerner fundamentally shifted the EHR landscape, creating both opportunities and uncertainties that traditional vendor evaluations often miss.
This isn't about helping organizations "switch" from Cerner. Instead, we're exploring the strategic value of Cerner's high-level modules, integration capabilities, and platform potential for three critical use cases: outpatient practice consolidation, custom development projects, and third-party system integration.
For CTOs and CIOs at PE-backed organizations, understanding Cerner's post-acquisition trajectory is essential for making technology investments that align with 3-5 year exit strategies. This comprehensive assessment provides the executive-level analysis you need to make informed decisions about Oracle Health EHR implementation, integration, or expansion.
Executive Summary: Cerner's Current Market Position
Oracle Acquisition Status and Strategic Implications
Oracle's $28.3 billion acquisition of Cerner fundamentally reshaping the EHR landscape. The acquisition represents Oracle's largest deal ever and positions the combined entity as a formidable healthcare technology platform. For PE-backed healthcare organizations, this acquisition introduces both opportunities and uncertainties that require careful strategic evaluation.
The integration has been marked by significant organizational changes, including rebranding Cerner as Oracle Health and appointing new leadership. David Feinberg, MD, now serves as chair of Oracle Health, while Seema Verma oversees Oracle's life sciences business, signaling Oracle's commitment to healthcare transformation.
2025 Market Share Analysis: Competitive Positioning
Oracle Health currently holds 22.9% of the acute care EHR market, down from 25% in 2021. This decline reflects competitive pressure from Epic, which has grown to 42.3% market share through consistent customer wins and retention.
The market dynamics are concerning for Oracle Health. In 2024, the company lost 74 hospitals and 17,232 beds, while Epic added 176 facilities and 29,399 beds. Notably, Oracle declined to share new contract data with KLAS Research for the first time, suggesting strategic sensitivity around market performance.
Key Changes Affecting Prospective Customers
Product Roadmap Shifts
Oracle has announced a next-generation cloud-native EHR scheduled for 2025, incorporating:
- Oracle's Clinical AI Agent
- Voice navigation
- Oracle Cloud Infrastructure
However, implementation delays have plagued current Cerner deployments, including indefinite postponements at Airedale NHS Foundation Trust and Sheffield Teaching Hospitals.
Support Model Changes
Customer organizations report challenges with "poor partnership and a lack of follow-through on promises" from Oracle Health. The transition period has created uncertainty around support quality and vendor responsiveness.
Pricing Structure Evolution
Oracle has implemented simplified contract models spanning the entire relationship across all offerings, potentially affecting long-term cost predictability for multi-year PE investment horizons.
Bottom-Line Recommendation Framework
For PE-backed healthcare organizations, Oracle Health presents a cautious opportunity requiring careful due diligence:
Consider Oracle Health if:
- Your investment timeline exceeds 5 years, allowing time for Oracle's platform modernization
- You require strong ambulatory capabilities where Oracle maintains competitive positioning
- Your organization needs deep interoperability with Oracle's enterprise systems
- Your portfolio includes multiple Oracle installations that could benefit from standardization
Exercise caution if:
- You require immediate implementation within 18-24 months
- Your exit strategy depends on seamless technology transitions
- You're competing directly with Epic-enabled health systems
- Your due diligence reveals implementation delays at comparable organizations
Post-Oracle Acquisition Impact Analysis
Timeline of Changes Since 2022 Acquisition
Phase 1: Integration and Rebranding (June 2022 - December 2022)
Oracle immediately began rebranding Cerner as Oracle Health and installed new leadership. The company appointed David Feinberg, MD, as chair and Travis Dalton as general manager of government services, signaling strategic focus on federal healthcare markets.
Phase 2: Product Development and AI Integration (2023-2024)
Oracle launched the Clinical AI Agent (formerly Clinical Digital Assistant), a voice-activated tool
that generates clinical notes and suggests follow-up actions. The company also introduced Seamless Exchange, an interoperability tool consolidating patient data from various sources.
Phase 3: Market Challenges and Strategic Pivots (2024-Present)
Despite technological advances, Oracle Health has faced significant market share losses and
implementation challenges. The company's response includes announcing a completely new EHR platform for 2025 and pursuing QHIN status under TEFCA for enhanced interoperability.
Product Roadmap Shifts and Investment Priorities
Oracle's next-generation EHR announcement in October 2024 represents a fundamental strategic shift. The new platform incorporates:
- AI-First Architecture: Deep integration of Oracle's Clinical AI Agent with voice-activated navigation
- Cloud-Native Design: Built entirely on Oracle Cloud Infrastructure for scalability and performance
- Simplified User Experience: Elimination of traditional menus in favor of voice commands and intuitive workflows
This roadmap shift creates both opportunity and risk for PE-backed organizations. While the new platform promises significant technological advancement, it effectively acknowledges limitations in the current Millennium platform that many customers depend on.
Support Model Changes and Operational Impact
The acquisition has fundamentally altered Cerner's support model, with mixed results for customers. More than half of interviewed clients using Cerner's implementation and IT advisory services report dissatisfaction, compared to higher satisfaction rates with third-party implementation partners.
Oracle's internal reorganization has created service delivery challenges:
- Consultant turnover during the transition has disrupted ongoing projects
- Process standardization efforts have sometimes conflicted with customer-specific needs
- Support escalation paths have changed, affecting issue resolution timelines
Oracle Cloud Infrastructure Integration Requirements
Oracle Health's strategic direction increasingly emphasizes Oracle Cloud Infrastructure (OCI) integration. For PE-backed organizations, this creates both technical requirements and strategic dependencies:
Technical Requirements:
- Network connectivity and bandwidth requirements for cloud-based services
- Security protocols alignment with Oracle's cloud security model
- Data migration capabilities for existing on-premise installations
- Integration architecture supporting hybrid cloud deployments
Strategic Implications:
- Vendor lock-in considerations as Oracle tightens platform integration
- Cost structure changes from capital expenditure to operational expenditure models
- Scalability benefits for organizations planning rapid growth or acquisitions
- Exit complexity for PE firms considering portfolio company sales to non-Oracle environments
Customer Retention Rates and Satisfaction Metrics
Market data reveals concerning trends in Oracle Health customer satisfaction and retention:
Customer Satisfaction Scores:
- 52% customer satisfaction score, compared to 66% for competitor McKesson
- Net Promoter Score of -18 with 51% detractors
- Only 9% of surveyed customers reported feeling highly satisfied with Cerner EHR in 2023
Market Performance:
- Net loss of 74 hospitals in 2024 representing continued market share erosion
- Revenue cycle management concerns with customers reporting poor communication and reliability issues
- Interoperability performance scored C+ grade from customers in 2023 assessments
However, Oracle Health maintains strengths in specific areas:
- Telehealth suite recognition through Cerner-Amwell collaboration
- KLAS recognition for acute care EMR in Middle East and Africa for six consecutive years
- Ambulatory surgery center success with documented patient satisfaction improvements
Cerner EHR Core Capabilities & Technical Architecture
Electronic Health Record Functionality Overview
Oracle Health EHR (formerly Cerner Millennium) provides comprehensive electronic health record functionality across multiple care settings. The platform consists of two primary architectures serving different organizational needs:
Cerner Millennium represents the flagship enterprise platform with 2.24% market share in the EHR category, serving 642 customers globally. Millennium offers robust clinical functionality including patient management, clinical documentation, order entry, and decision support tools. The platform is praised for its interoperability with other systems and comprehensive reporting capabilities.
Cerner Soarian serves as a specialized solution with 0.12% market share and 32 customers. Soarian is known for its user-friendly interface and faster user adoption rates, though it lacks some advanced analytics capabilities compared to Millennium. Note, they are transitioning away from Soarian.
SMART on FHIR Capabilities and API Ecosystem
Oracle Health provides extensive FHIR R4 API support through the Oracle Health Millennium Platform. The implementation follows HL7 FHIR 4.0.1 specification and supports both open and secured endpoints.
API Limitations: Important for PE-backed organizations to understand that Oracle's FHIR APIs are primarily read-only, with limited write capabilities. Organizations cannot use these APIs for placing orders or real-time bidirectional data synchronization.
Interoperability Features and Third-Party Integrations
Oracle Health emphasizes open systems interoperability to support healthcare ecosystem connectivity. The platform provides multiple integration pathways:
Industry Standards Support:
- HL7 Integration: Comprehensive support for HL7 v2.3.1 through v2.9 standards
- FHIR Implementation: Both DSTU2 and R4 versions with December 2025 DSTU2 end-of-support
- C-CDA Compatibility: Clinical Document Architecture support for care transitions
- Direct Messaging: Secure clinical information exchange capabilities
Enterprise Integration Capabilities:
- Oracle Integration for Healthcare enables organizations to create healthcare-specific integrations
- CommonWell Health Alliance: Oracle Health participates in this network facilitating record exchange for 171 million individuals
- TEFCA Participation: Oracle Health Information Network is pursuing QHIN status for standardized health data sharing
Oracle Health Seamless Exchange: This proprietary solution aggregates external health data from multiple sources to create comprehensive patient records. The system includes advanced deduplication capabilities and allows organizations to designate trusted sources for automatic data integration.
Data Warehouse and Analytics Capabilities
Oracle Health's analytics architecture centers on Oracle Health Data Intelligence (formerly HealtheIntent), providing a modular suite of cloud applications and analytics services. The platform enables healthcare organizations to leverage data for improved patient outcomes and operational efficiency.
Analytics Platform Features:
- Population Health Management: Tools for risk stratification and coordinated care programs
- Clinical Quality Measurement: Automated quality reporting and performance tracking
- Operational Analytics: Resource optimization and workflow analysis capabilities
- Predictive Analytics: Machine learning capabilities for patient risk assessment
Oracle Health Advance: This specialized analytics suite compares clinician efficiency and adoption patterns across peer networks. The platform provides:
- Efficiency Benchmarking: Individual clinician performance compared to national peers
- ROI Analysis: Specific project identification with quantified return on investment
- Usage Pattern Analysis: Behavioral insights for targeted training and optimization
Cloud Migration Readiness and Infrastructure Requirements
Oracle Health's strategic direction emphasizes Oracle Cloud Infrastructure (OCI) as the foundation for all future healthcare deployments. The platform provides multiple deployment options to accommodate different organizational needs:
Oracle Cloud Infrastructure Benefits:
- Autonomous Shield Initiative: Oracle offers simplified EHR migrations to OCI at no additional cost for existing Oracle Health customers
- Healthcare-Optimized Infrastructure: Purpose-built cloud services for healthcare workloads including HIPAA compliance and healthcare-specific security controls
- Global Availability: Oracle Cloud regions worldwide supporting international healthcare operations
Hybrid Deployment Options:
- On-Premise Integration: Maintained support for existing on-premise Millennium installations
- Cloud Migration Pathways: Structured migration approaches from legacy systems to OCI
- Multi-Cloud Support: Oracle Integration services support connections to multiple cloud platforms
The platform's cloud readiness represents both an opportunity and a dependency consideration for PE-backed organizations. While OCI provides enterprise-grade infrastructure capabilities, organizations must evaluate the long-term implications of deeper Oracle platform integration for future flexibility and exit strategies.
PE-Backed Organization Strategic Considerations
Implementation Timelines Aligned with 3-5 Year Exit Strategies
PE firms operating on typical 3-5 year investment horizons face critical timing considerations with Oracle Health implementations. Oracle estimates 15 months or longer for each facility in large hospital systems, including full clinical functionality, revenue cycle products, and post-implementation optimization.
Timeline Reality Check
- Small practices (1-10 providers): 6-12 months for basic implementation
- Mid-size organizations (11-50 providers): 12-18 months including training and optimization
- Large health systems (100+ providers): 18-36 months for comprehensive deployment
Recent implementation challenges compound timing risks. Multiple Oracle Health deployments have experienced significant delays, including indefinite postponements at major health systems. The Department of Veterans Affairs paused Oracle Health deployments in April 2023 for a comprehensive reset, with restart planned for mid-2026.
PE Timeline Optimization Strategies
- Phased Implementation: Deploy core modules first with advanced features in subsequent phases
- Third-Party Implementation Partners: KLAS reports higher satisfaction with third-party firms compared to Oracle's internal services
- Exit Planning Integration: Align EHR selection with buyer preferences in target markets
Scalability for Multi-Site Rollups and Acquisitions
Oracle Health's architecture provides advantages for PE portfolio companies executing roll-up strategies. The platform's modular design supports both cloud and on-premise deployments, accommodating diverse acquisition integration scenarios.
Multi-Site Deployment Advantages:
- Standardized Workflows: Oracle Health supports more than 55 medical specialties with consistent user interfaces
- Centralized Administration: Single platform management across multiple locations
- Acquisition Integration: Oracle's simplified contract model can accommodate rapid acquisition integration
Case Study Evidence: Private equity healthcare platforms report success with Oracle Health for acquisition integration. One PE-backed organization completed four acquisitions with Oracle Fusion integration in 4-5 months, demonstrating scalability for roll-up strategies.
Due Diligence Implications for Potential Buyers
Oracle Health implementations create specific considerations for eventual portfolio company exits. Strategic and financial buyers increasingly evaluate healthcare technology infrastructure as a key valuation factor.
Buyer Perspective Considerations:
- Platform Standardization: Oracle Health provides unified technology stack attractive to strategic buyers
- Integration Complexity: Epic-dominated health systems may prefer Epic-standardized acquisitions
- Total Cost of Ownership: Long-term Oracle platform costs may affect buyer valuations
Due Diligence Focus Areas:
- Implementation Status: Document completion rates and optimization levels
- User Satisfaction: Current satisfaction scores of 52% may indicate training needs
- Contract Terms: Oracle's contract structure and future pricing commitments
- Technical Debt: Legacy system integration status and modernization requirements
Total Cost of Ownership Analysis for Operational Efficiency Goals
PE firms require comprehensive TCO analysis encompassing implementation, operations, and exit considerations. Oracle Health pricing varies significantly based on organizational size and module requirements.
Implementation Cost Breakdown:
- Small practices (1-10 providers): $10,000-$200,000 implementation with $1,000-$3,000 monthly per provider
- Mid-sized organizations (11-50 providers): $150,000-$500,000 implementation with $75,000-$120,000 annual maintenance
- Large health systems (100+ providers): $800,000-$5 million implementation with $400,000-$3 million annual maintenance
Ongoing Cost Components:
- Base Software Licensing: $25 per user per month for cloud-based deployments
- Customization Costs: $1,000-$1,000,000 depending on organizational complexity
- Third-Party Integration: Additional costs for specialty applications and interfaces
- Cloud Infrastructure: Oracle Cloud Infrastructure costs for hosted deployments
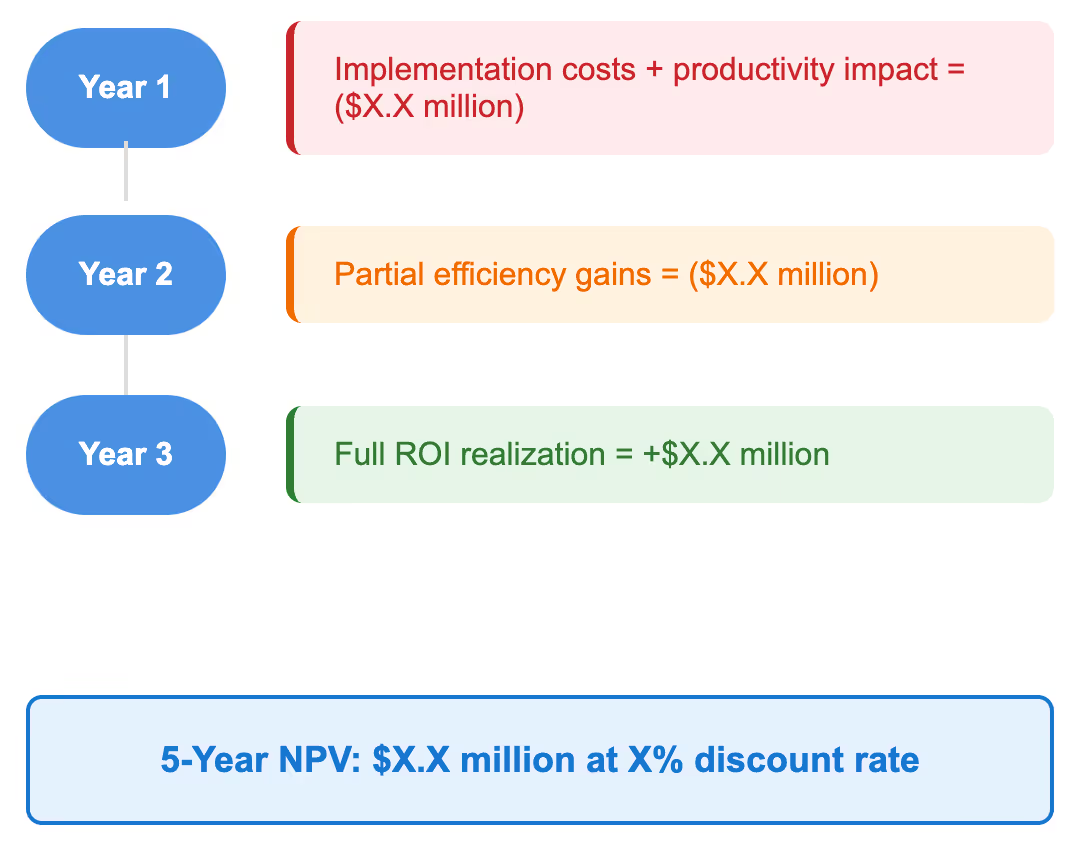
EBITDA Impact During Implementation Phases
Oracle Health implementations significantly impact EBITDA during deployment phases, requiring careful financial planning and change management.
Implementation Phase EBITDA Impacts:
- Months 1-6: Negative impact from staff training, temporary productivity decline, and implementation costs
- Months 6-12: Continued investment with gradual productivity recovery
- Months 12-24: Positive impact realization through workflow optimization and efficiency gains
Mitigation Strategies:
- Phased Rollout: Minimize operational disruption through staged deployment
- Change Management Investment: Dedicated training and support resources to accelerate adoption
- Productivity Monitoring: Real-time tracking of key performance indicators during transition
PE firms should budget for 12-18 month EBITDA impact periods with positive returns typically materializing in the second year post-implementation. Organizations with effective change management and implementation partners often achieve faster positive impact realization.
Competitive Analysis: Cerner vs Epic vs Alternatives
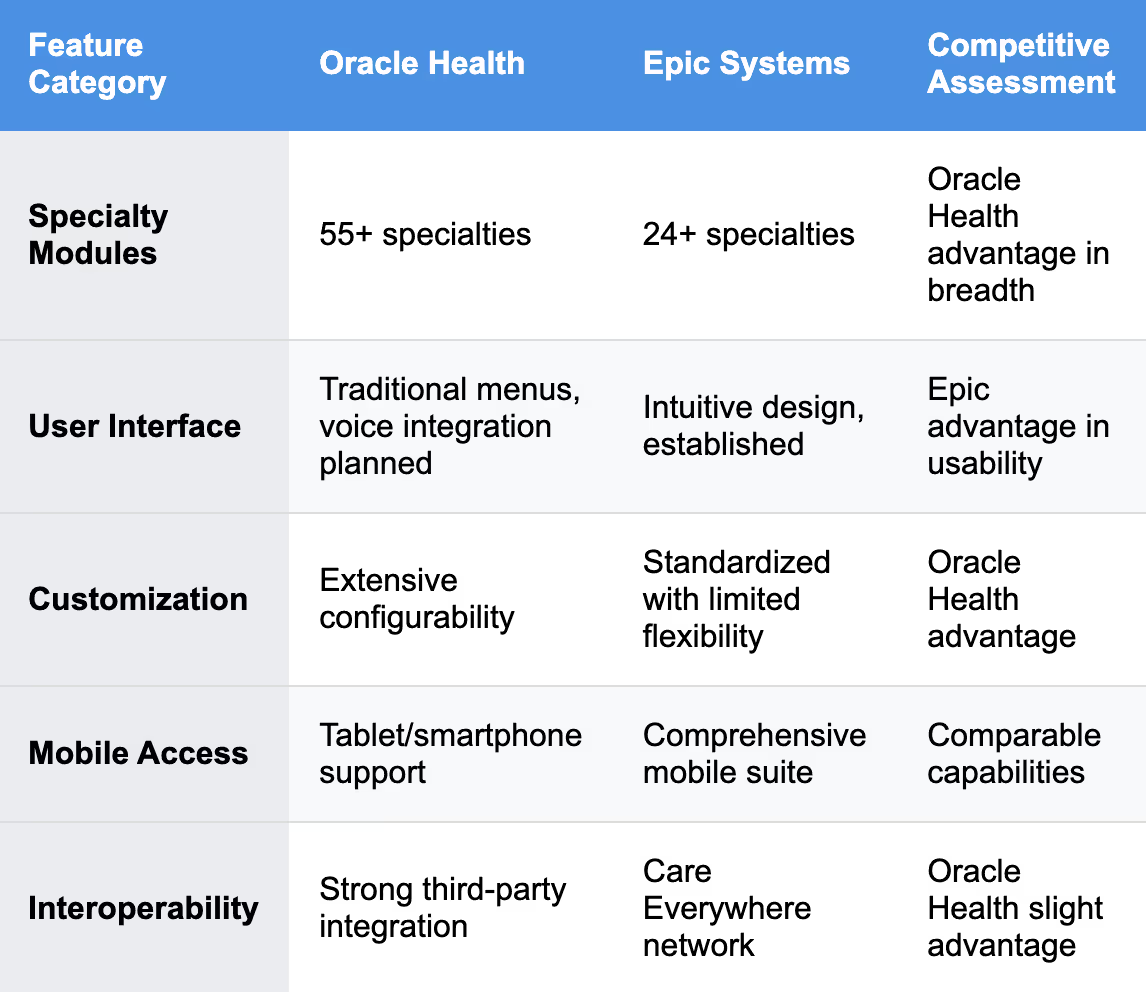
Feature-by-Feature Comparison with Major Competitors
Oracle Health competes directly with Epic Systems, which currently dominates the market with 42.3% market share compared to Oracle Health's 22.9%. The competitive landscape reveals distinct strengths and weaknesses across major platforms.
Technical Architecture Differences
- Oracle Health: Built on Oracle Database with MUMPS/Chronicles foundation, offering robust database capabilities but legacy constraints
- Epic: Purpose-built healthcare architecture with tight integration across modules, prioritizing workflow optimization over technical flexibility
- Meditech: Cost-effective alternative with 13.2% market share, particularly strong in smaller hospitals
Implementation Complexity Rankings and Success Metrics
Implementation complexity varies significantly across EHR platforms, with important implications for PE-backed organizations operating under time constraints.
Implementation Complexity Assessment
Epic Systems:
- Average Timeline: 18-24 months for large health systems
- Cost Range: $1,200-$500,000 per provider
- Success Rate: High customer satisfaction but significant resource requirements
- Training Requirements: Extensive certification programs with $2,000+ per organization
- Hiring Note: Very easy to hire Epic vendors
Oracle Health:
- Average Timeline: 15+ months per facility
- Cost Range: $25-$3,000 per provider monthly
- Success Rate: More than half of Oracle implementation clients report dissatisfaction
- Training Requirements: Flexible training options with third-party support
Implementation Risk Factors:
- Oracle Health: Recent implementation delays at major health systems create timeline uncertainty
- Epic: Resource-intensive implementation but proven track record at large organizations
- Meditech: Faster implementation but limited advanced functionality
Specialty-Specific Capabilities (Outpatient/Clinic Settings)
For PE-backed organizations focusing on ambulatory and outpatient settings, specialty-specific capabilities become critical differentiators.
Oracle Health Ambulatory Strengths:
- Ambulatory Surgery Center optimization with demonstrated ROI improvements
- Specialty workflow support for over 55 medical specialties
- Revenue cycle integration through Oracle's comprehensive platform
- Modular deployment allowing focused implementation on specific practice areas
Market Performance Data:
- Oracle Health holds 25.06% of ambulatory EHR market compared to Epic's 43.92%
- Ambulatory surgery centers report significant benefits, including reduced complications and improved patient satisfaction
Competitive Positioning:
- Epic: Stronger in large integrated delivery networks but limited ambulatory-specific features
- Oracle Health: Better suited for independent practices and specialty clinics
- athenahealth: Specialized ambulatory focus with practice management integration
KLAS Customer Satisfaction Scores and Peer Feedback
KLAS Research provides objective customer satisfaction data crucial for PE due diligence processes.
Oracle Health KLAS Performance:
- Overall performance varies by segment with some product categories showing insufficient data for ranking
- Revenue Cycle Management: Customer satisfaction trending down since 2018 with 21% decrease in satisfaction
- Implementation Services: Oracle's internal services underperform third-party alternatives
Comparative KLAS Rankings (2025 Best in KLAS):
- Epic: Top Overall Health System Suite for fifteenth consecutive year
- Oracle Health: Third place after Epic and Meditech in overall rankings
- athenahealth: Top independent physician practice suite
Customer Feedback Themes:
- Positive: Strong interoperability, comprehensive specialty support, ambulatory capabilities
- Negative: Implementation challenges, revenue cycle complexity, inconsistent support quality
- Neutral: Platform functionality adequate but user experience behind market leaders
Integration Capabilities and Vendor Ecosystem Strength
Oracle Health's integration ecosystem represents both a strength and a strategic consideration for PE-backed organizations.
Oracle Health Integration Advantages:
- Open API Policy extending support to competitors through comprehensive integration capabilities
- Industry Standards Support: HL7, FHIR, and CDA standards compliance exceeding Epic's interoperability
- Oracle Enterprise Integration: Seamless connectivity with Oracle's business applications suite
- Third-Party Ecosystem: Oracle Health Developer Program supporting extensive integration development
Epic Integration Comparison:
- Care Everywhere Network: Proprietary but widely adopted interoperability platform
- App Orchard: Extensive third-party application marketplace
- Standardized APIs: FHIR implementation focused on core clinical workflows
- Closed Ecosystem: More restrictive but more controlled integration environment
Strategic Ecosystem Considerations:
- Oracle Dependence: Deeper integration with Oracle platform creates vendor lock-in risks
- Market Network Effects: Epic's larger market share creates broader interoperability benefits
- Innovation Velocity: Oracle's enterprise focus may accelerate healthcare innovation through enterprise technologies
For PE-backed organizations, the choice between Oracle Health and competitors ultimately depends on specific portfolio strategy, exit timeline, and target market characteristics. Oracle Health offers advantages for organizations requiring deep customization, ambulatory focus, or Oracle enterprise integration, while Epic provides market leadership and proven large-scale implementation success.
Implementation Reality Check: Costs, Timelines & Resources
Average Implementation Timeline by Organization Size
Oracle Health implementations vary significantly based on organizational complexity, requiring realistic timeline planning for PE investment strategies.
Small Practices (1-10 Providers)
- Timeline: 6-12 months including training and optimization
- Key Phases: System configuration (2-3 months), data migration (1-2 months), training (2-3 months), go-live support (1-2 months)
- Critical Success Factors: Dedicated project management and realistic workflow documentation
Mid-Size Organizations (11-50 Providers)
- Timeline: 12-18 months for comprehensive deployment
- Key Phases: Requirements gathering (2-3 months), system build (3-4 months), integration testing (2-3 months), training (3-4 months), optimization (2-3 months)
- Critical Success Factors: Executive sponsorship and change management throughout implementation
Large Health Systems (100+ Providers)
- Timeline: 15+ months per facility including full clinical functionality and revenue cycle integration
- Key Phases: Planning and design (3-6 months), configuration and build (6-9 months), testing and validation (3-6 months), deployment and optimization (6-12 months)
- Critical Success Factors: Dedicated implementation team and staged rollout approach
Implementation Methodology Changes: Oracle has transitioned from waterfall to agile TIP (The Iterative Process) methodology, using workshop-based design sessions. While this approach can accelerate certain phases, it makes precise hour estimation more challenging for project planning.
Resource Requirements and Internal Team Impact
Oracle Health implementations require substantial internal resource commitments that PE firms must factor into portfolio company budgeting and staffing plans.
Core Implementation Team Requirements
- Executive Sponsor: C-level executive with decision-making authority and organizational influence
- Project Manager: Dedicated PM with healthcare IT experience
- Clinical Champions: Physician and nursing leaders from each department
- IT Resources: Systems administrators and technical specialists
- Training Coordinators: Dedicated staff for user training and support
Internal Staff Impact During Implementation
- Productivity Decline: Expect 15-25% productivity reduction during training and go-live phases
- Overtime Requirements: Clinical staff often work additional hours completing documentation during transition
- Learning Curve: High learning curve for new users requiring sustained training support
- Change Management: Significant organizational culture adaptation required
Hidden Costs and Budget Planning Considerations
PE firms must account for implementation costs beyond vendor licensing that can significantly impact total investment requirements.
Direct Hidden Costs
- Third-Party Integration: $25,000-$100,000+ per interface for complex system connections
- Data Migration Services: $50,000-$1,000,000+ for legacy system data conversion
- Customization Requirements: $10,000-$1,000,000 depending on organizational complexity
- Infrastructure Upgrades: Hardware, network, and security improvements for Oracle Health compatibility
- Backup and Disaster Recovery: Enhanced systems for protecting clinical data
Indirect Cost Factors
- Consultant Fees: Third-party implementation partners often outperform Oracle's internal services
- Travel and Training: Staff certification and on-site training expenses
- Temporary Staffing: Additional clinical staff during transition periods
- Lost Productivity: Revenue impact during implementation phases
- Opportunity Costs: Delayed strategic initiatives during EHR focus period
Cost Example: A 200-bed hospital typically invests $2-5 million in Oracle Health implementation, with annual maintenance costs of $150,000-$1 million ongoing.
Change Management and Training Requirements
Successful Oracle Health implementations require comprehensive change management programs addressing both technical and cultural transformation.
Training Program Components
- Leadership Training: Executive and physician leader preparation for organizational change
- End-User Training: Role-specific training for clinical and administrative staff
- Super-User Development: Advanced training for internal support champions
- Ongoing Education: Continuous learning programs for new features and optimization
Oracle Health Training Approaches
- Simulation Training: Hands-on practice in test environments before go-live
- Workflow-Based Training: Training organized around actual patient care processes
- Just-in-Time Training: Immediate support during early system use
- Competency Validation: Formal assessment of user proficiency before independent system use
ROI Timelines and Operational Efficiency Gains
PE firms require clear ROI timelines to evaluate Oracle Health investments against alternative capital allocation options.
Typical ROI Timeline
- Months 1-6: Negative ROI due to implementation costs and productivity decline
- Months 6-12: Break-even period as staff proficiency improves
- Months 12-24: Positive ROI realization through operational efficiency gains
- Months 24+: Sustained ROI through optimized workflows and reduced administrative costs
Operational Efficiency Metrics
- Clinical Documentation: 20-30% reduction in documentation time through templates and automation
- Medication Safety: Reduced adverse drug events through integrated decision support
- Care Coordination: Improved information sharing across care teams and departments
- Regulatory Compliance: Automated reporting reducing manual compliance efforts
ROI Calculation Example
For a $3 million Oracle Health implementation at a 300-bed hospital:
- Year 1: -$3.5 million (implementation costs + productivity loss)
- Year 2: -$500,000 (continuing optimization + efficiency gains beginning)
- Year 3: +$1.2 million (full efficiency realization)
- 5-Year Net ROI: 180% assuming continued operational benefits
PE firms should plan for 24-36 month positive ROI timelines with the understanding that successful implementations require sustained organizational commitment and adequate resource allocation throughout the implementation period.
Strategic Decision Framework for Healthcare CTOs
Evaluation Criteria Matrix for EHR Vendor Selection
Healthcare CTOs in PE-backed organizations require systematic evaluation frameworks that balance technical capabilities with investment timeline constraints and strategic objectives.
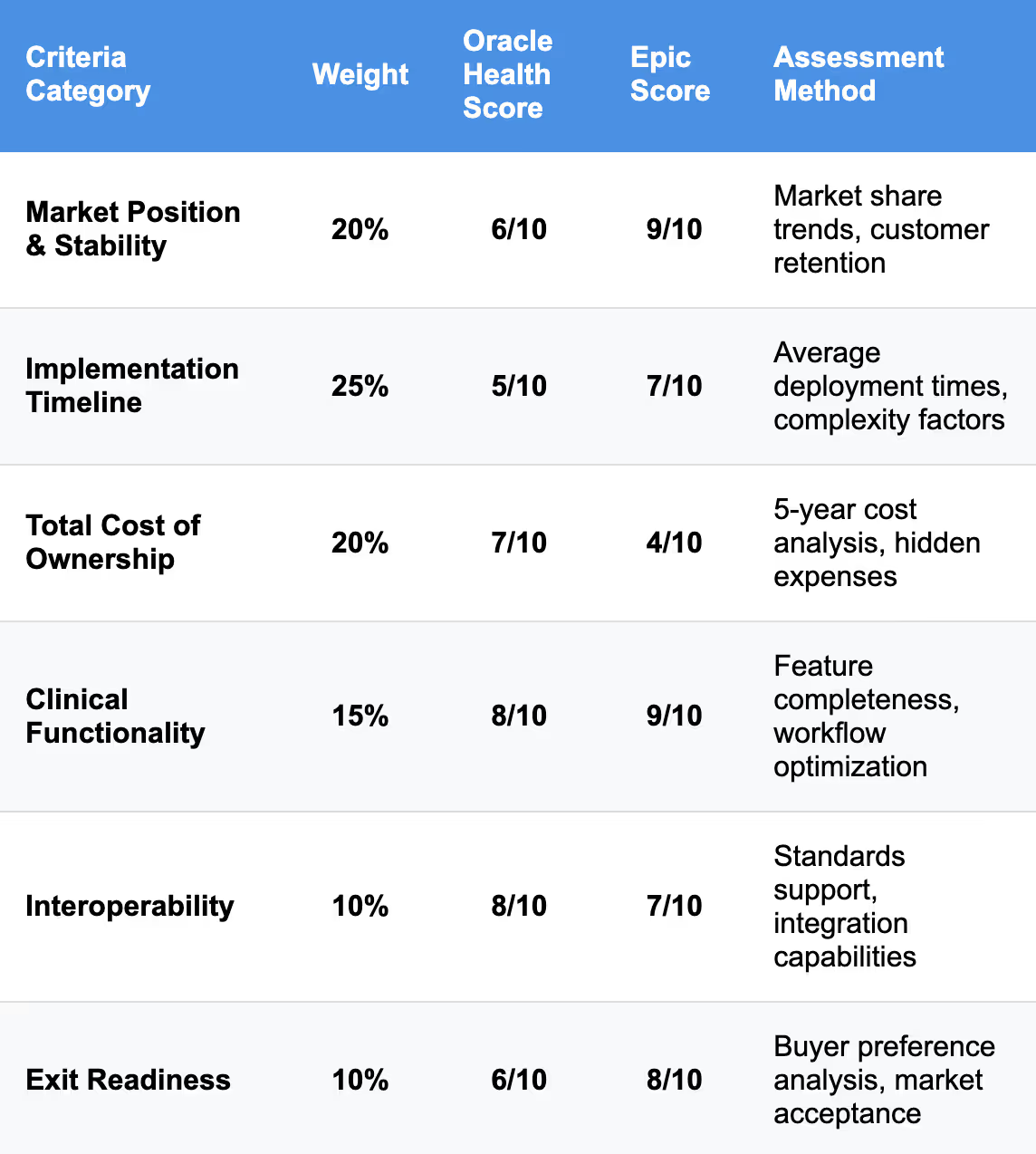
PE-Specific Evaluation Criteria
- Implementation Speed: Ability to complete deployment within PE holding period
- Scalability: Support for rapid growth and acquisition integration
- Exit Enhancement: Platform attractiveness to potential strategic buyers
- EBITDA Impact: Timeline for positive financial contribution
- Risk Mitigation: Implementation success probability and contingency options
Risk Assessment Methodology for Oracle-Dependent Solutions
Oracle's acquisition of Cerner creates specific risk factors that CTOs must evaluate systematically.
Technology Risk Assessment
Platform Evolution Risk: Oracle's next-generation EHR creates uncertainty around current platform investment longevity. Organizations implementing current Oracle Health technology face potential migration requirements within 3-5 years.
Vendor Lock-in Risk: Oracle's strategy increasingly emphasizes Oracle Cloud Infrastructure integration, potentially creating deeper technology dependencies that complicate future vendor changes or portfolio company exits.
Implementation Risk: Recent deployment challenges, including indefinite postponements at major health systems, suggest elevated implementation risk requiring robust contingency planning.
Risk Mitigation Strategies
- Phased Implementation: Deploy core functionality first with advanced features contingent on Oracle's platform stability
- Third-Party Implementation Partners: According to KLAS, there’s higher satisfaction with third-party firms compared to Oracle's internal services
- Contract Protection: Negotiate milestone-based payments and performance guarantees
- Exit Planning: Include EHR platform considerations in strategic buyer identification and valuation discussions
Migration Pathway Analysis from Legacy Systems
CTOs must develop comprehensive migration strategies that minimize operational disruption while maximizing strategic value.
Legacy System Assessment Framework
Data Migration Complexity:
- Clinical Data: Patient records, lab results, imaging studies, and medication histories
- Financial Data: Billing history, insurance information, and accounts receivable
- Operational Data: Scheduling, inventory, and administrative records
- Integration Points: Existing system connections requiring replacement or modification
Migration Pathway Options
Big Bang Migration: Complete cutover to Oracle Health with legacy system shutdown
- Advantages: Faster completion, no dual-system maintenance
- Disadvantages: Higher risk, significant staff disruption
- Recommended For: Smaller organizations with simpler technology environments
Phased Migration: Gradual transition with parallel system operation
- Advantages: Lower risk, manageable change pace
- Disadvantages: Extended timeline, dual-system costs
- Recommended For: Larger organizations with complex integration requirements
Hybrid Approach: Core clinical functions migrate first with administrative systems following
- Advantages: Balanced risk and timeline
- Disadvantages: Complex integration management
- Recommended For: Most PE-backed organizations seeking optimized risk-return balance
Board Presentation Template and Executive Summary Points
PE-backed healthcare CTOs require board-ready analysis frameworks that align technical decisions with investment strategy.
Executive Summary Template
Strategic Recommendation: [Clear recommendation with supporting rationale]
Investment Summary:
- Total Investment Required: [Implementation + infrastructure + contingency costs]
- Timeline: [Deployment schedule aligned with holding period]
- ROI Timeline: [Break-even and positive return projections]
- Risk Assessment: [Key risks and mitigation strategies]
Business Case Framework
Market Position Analysis:
- Oracle Health market share trends and competitive position
- Strategic buyer preference assessment in target markets
- Platform longevity and evolution roadmap implications
Financial Impact Modeling
Board Decision Framework
Proceed with Oracle Health if:
- Investment timeline exceeds 5 years allowing platform maturation
- Portfolio includes other Oracle enterprise systems
- Ambulatory/specialty clinic focus aligns with Oracle Health strengths
- Budget accommodates potential implementation delays
Consider Alternatives if:
- Exit timeline requires implementation completion within 24 months
- Strategic buyers predominantly use Epic or other platforms
- Organization requires immediate deployment certainty
- Budget constraints limit implementation contingency planning
Real-World Case Studies: PE-Backed Cerner Implementations
Implementation Success Stories and Lessons Learned
Real-world implementation experiences provide crucial insights for PE-backed organizations evaluating Oracle Health investments.
Ambulatory Surgery Center Success
An American Surgery Center in Delaware founded in 2015 demonstrates Oracle Health's value proposition for specialty care settings. The organization replaced inefficient paper-based systems with Oracle Health EHR, achieving significant operational improvements:
- Workflow Optimization: Integrated scheduling, documentation, and billing processes
- Quality Improvements: Enhanced patient safety through standardized protocols
- Staff Efficiency: Reduced administrative burden allowing focus on patient care
- Scalability: Technology platform supporting growth and potential acquisition appeal
Key Success Factors Identified:
- Executive Leadership: Strong commitment from ownership through implementation challenges
- Workflow Focus: Emphasis on optimizing surgical processes rather than just technology deployment
- Staff Engagement: Comprehensive training ensuring user adoption and proficiency
Mid-Size Hospital Implementation
A case study from MedSys Group demonstrates Oracle Health's capabilities for complex multi-system environments. The project involved a 270-bed hospital and 15 associated clinics replacing Soarian clinical systems with Cerner Millennium while maintaining Soarian Financials:
- Hybrid Approach: Leveraged existing financial system investment while upgrading clinical capabilities
- Phased Implementation: Managed complexity through structured deployment timeline
- Change Management: Professional implementation support throughout 18-month project timeline
Enterprise Healthcare Platform
Omega Healthcare's experience illustrates Oracle's capabilities for PE-backed platform growth. This healthcare solutions provider used Oracle Fusion Cloud applications to manage multiple acquisitions:
- Rapid Integration: Completed four acquisitions with backend integration in 4-5 months
- Scalability: Supported growth from 10,000 to 35,000 employees
- Operational Efficiency: Reduced quarterly financial close from 25 days to 2 days
- Unified Platform: Single technology stack across all acquired entities
Post-Implementation Operational Improvements
Documented operational improvements provide ROI validation for PE investment committees.
Clinical Quality Metrics
- Patient Safety: One ambulatory surgery center reduced complications from 32% to 26.5% after Oracle Health implementation
- Documentation Quality: Standardized clinical documentation improving care continuity
- Medication Safety: Reduced adverse drug events through integrated decision support
- Care Coordination: Enhanced information sharing across departments and specialties
Operational Efficiency Gains
- Administrative Efficiency: Reduced time spent on manual documentation and information retrieval
- Revenue Cycle Performance: Improved billing accuracy and reduced claim denials
- Regulatory Compliance: Automated reporting reducing manual compliance efforts
- Staff Productivity: Streamlined workflows allowing focus on patient care
Financial Performance Impact
- Revenue Enhancement: Better capture of billable services through improved documentation
- Cost Reduction: Elimination of paper records and manual processes
- Quality Bonuses: Improved performance in value-based care contracts
- Operational Leverage: Technology platform supporting growth without proportional staff increases
Exit Readiness Implications and Buyer Perspectives
PE firms must consider how Oracle Health implementations affect portfolio company exit strategies and buyer appeal.
Strategic Buyer Considerations
- Technology Standardization: Oracle Health provides unified platform attractive to acquirers with existing Oracle investments
- Integration Complexity: Epic-dominated health systems may prefer Epic-standardized acquisitions
- Market Position: Oracle Health's declining market share may affect buyer perceptions
- Platform Maturity: Oracle's next-generation EHR announcement suggests current platform limitations
Financial Buyer Perspectives
- Operational Efficiency: Well-implemented Oracle Health systems demonstrate operational optimization
- Scalability: Platform supports additional growth and acquisition integration
- Technology Investment: Recent implementation reduces future capital requirements
- Risk Assessment: Implementation history and user satisfaction affect valuation
Exit Preparation Strategies
- Documentation: Comprehensive implementation records and performance metrics
- Optimization: Ensure system utilization maximizes operational benefits
- Integration Assessment: Evaluate compatibility with potential strategic acquirer platforms
- Contract Review: Understand ongoing commitments and migration options
Organizations achieving successful Oracle Health implementations typically receive positive buyer reception when:
- Operational metrics demonstrate clear efficiency gains and quality improvements
- Staff satisfaction indicates successful technology adoption
- Financial performance shows measurable ROI from technology investment
- Strategic positioning aligns with buyer technology preferences
Final Takeaways
Oracle Health represents a compelling but complex solution for healthcare organizations, particularly those focused on outpatient practice consolidation, custom development projects, or complex system integration requirements. Oracle's acquisition has strengthened the platform's technical capabilities while introducing new considerations around support models and cloud infrastructure requirements.
The strategic value proposition centers on integration flexibility, modular implementation approaches, and Oracle-enhanced cloud capabilities. Organizations seeking to consolidate multiple practices, build custom clinical applications, or integrate with existing systems will find Oracle Health's architecture particularly well-suited to their requirements.
However, significant challenges must be acknowledged. Oracle Health's declining market share from 25% to 22.9% and customer satisfaction scores of only 52% create implementation and exit risks for PE-backed organizations. Recent deployment delays and indefinite postponements at major health systems compound timeline uncertainty.
Success requires understanding the post-acquisition landscape and aligning implementation strategies with organizational objectives. PE-backed organizations benefit from Oracle Health's scalability and operational efficiency potential, while technical organizations appreciate the platform's extensive API ecosystem and development capabilities.
The decision ultimately depends on specific organizational requirements, existing technology investments, and strategic growth objectives. Oracle Health's strengthened position post-acquisition makes it a viable long-term EHR solution for organizations prioritizing integration flexibility and cloud-native capabilities, provided they can navigate implementation challenges and timeline constraints.
For PE firms, Oracle Health represents a strategic technology investment requiring careful risk assessment and realistic timeline planning. Organizations should budget for extended implementation periods, invest heavily in change management, and maintain contingency plans for deployment challenges while positioning for long-term operational benefits.
Frequently Asked Questions
What are the main differences between Oracle Health and Epic for outpatient practices?
Oracle Health offers more flexible integration capabilities and modular implementation options, making it ideal for organizations seeking custom development or complex system integrations. Epic provides superior user experience and comprehensive functionality but requires more standardized implementation approaches. Oracle Health supports 55+ medical specialties compared to Epic's 24+ specialties, providing broader ambulatory coverage.
How has Oracle's acquisition affected pricing and implementation timelines?
Oracle has maintained existing pricing structures while introducing new cloud-based licensing options. Organizations can achieve cost optimization through Oracle Cloud Infrastructure integration, though implementation timelines have extended with Oracle estimating 15+ months per facility for comprehensive deployments. Recent delays at major health systems suggest longer timelines may be required.
What timeline should organizations expect for Oracle Health EHR implementation?
Implementation timelines range from 6-12 months for small outpatient practices to 15+ months for large health systems. However, recent implementation challenges including indefinite postponements suggest organizations should plan for extended timelines with robust contingency planning.
How does Oracle Health support practice consolidation and acquisition integration?
Oracle Health's modular architecture and simplified contract models facilitate rapid integration of acquired practices. One PE-backed organization completed four acquisitions with backend integration in 4-5 months using Oracle's platform, demonstrating scalability for roll-up strategies and multi-site consolidation.
What are the main risks of implementing Oracle Health for PE-backed organizations?
Key risks include declining market share potentially affecting buyer appeal, implementation delays extending beyond PE holding periods, and low customer satisfaction scores requiring significant change management investment. Organizations should evaluate third-party implementation partners and maintain realistic timeline expectations with contingency planning.
James founded Invene with a 20-year plan to build the world's leasing partner for healthcare innovation. A Forbes Next 1000 honoree, James specializes in helping mid-market and enterprise healthcare companies build AI-driven solutions with measurable PnL impact. Under his leadership, Invene has worked with 20 of the Fortune 100, achieved 22 FDA clearances, and launched over 400 products for their clients. James is known for driving results at the intersection of technology, healthcare, and business.
Ready to Tackle Your Hardest Data and Product Challenges?
We can accelerate your goals and drive measurable results.

