Why Healthcare Organizations Should Never Build a Custom EMR (And What Strategic Alternatives Actually Work)

If your leadership team is pushing for custom EMR development to solve high vendor costs or system limitations, you're walking into a potential $5-15 million mistake. Every month, fast-scaling clinic chains ask about building custom EMRs, and the answer is consistently the same: hell no.
Custom EMR projects fail spectacularly. Even sophisticated healthcare organizations like Intermountain Healthcare, after 40 years of successful homegrown EMR use, abandoned their custom system for commercial alternatives.
These clinics aren't product companies, and they consistently underestimate the complexity of building software from scratch while underbudgeting for iteration, support, and long-term maintenance.
This comprehensive analysis reveals why most healthcare organizations should avoid custom EMR development entirely, while providing strategic alternatives that address your real business needs without burning through capital.
Real Cost Breakdown That Boards Don't Discuss
The financial gulf between custom and commercial EMR solutions is staggering, and recent failures demonstrate just how catastrophic the cost overruns can become.
The average cost of custom EMR solutions is generally higher, coming in at around $2 million for mid-size organizations. But that's misleading. It's just the starting point before scope creep and complexity multiply costs.
A case study from Samsung Medical Center makes this clear. Its custom outpatient EMR, implemented in 2006–2008, produced a net present value of US$3.6 million and a benefit-cost ratio of 1.23 – but only after a 6.2-year payback period. Even in a successful deployment, leaders absorbed years of costs before realizing financial returns.
Meanwhile, commercial EMR solutions tend to deliver much more predictable upfront and ongoing costs. For small practices, base rates can be as low as $50-$300 per month. But required add-ons (telehealth, e-prescribing, and advanced modules) often push costs toward the upper end of that range.
Technical Complexity That Destroys Budgets and Timelines
The technical challenges extend far beyond coding. Modern EMRs often become bloated systems with poor standardization, especially around clinical documentation. Free-text SOAP notes create downstream data messes that AI must clean up, when EMRs should enforce structured data capture from the start.
Regulatory Compliance: The $500K-1M Annual Burden
Regulatory compliance represents one of the most underestimated costs in custom EMR development. Health systems running homegrown EMRs during the Meaningful Use era cited rising compliance costs as a key factor in replacing custom systems with commercial alternatives.
Intermountain Healthcare spent an estimated $12 million on custom modifications just to get federal certification in 2012, yet soon decided to replace its entire system with commercial Cerner. A single clinic cannot amortize compliance R&D costs the way large vendors serving hundreds of clients can.
Integration Ecosystem Challenges
The integration problem isn't just about custom EMRs. Vendors want to go complex and build out custom integrations, which makes everything harder. You're either going to get charged significantly more money for these custom integrations, or you're going to have to build the integrations internally.
This creates a lose-lose situation: pay premium rates for vendor-managed custom integrations, or hire developers to build and maintain integrations yourself. Either way, you're spending far more than expected on what should be standard connectivity.
The irony is that Epic and Cerner spent decades perfecting their integration networks, but they still charge premium rates for anything beyond basic connectivity. Every unique workflow or data exchange requirement becomes a custom project with custom pricing, making even commercial EMR implementations expensive integration nightmares.
Data Extraction and Analytics Challenges
Even if you can live with a commercial EMR's limitations, extracting data for analytics and compliance can be a nightmare. Existing platforms like Healthy or Athena make basic data extraction incredibly difficult, forcing organizations to either accept limited reporting capabilities or invest heavily in integration work to get their own data out.
This creates a false economy where organizations consider custom EMR development not because they need different functionality, but because they can't effectively use the data from their existing systems. The solution isn't rebuilding the entire EMR - it's implementing proper data integration and analytics overlays.
Feature Creep: How Projects Expand Beyond Control
Custom EMR projects suffer from uncontrolled scope expansion. The VA’s homegrown VistA system is a prime example. Originally designed as a lean, clinician-friendly EMR, VistA evolved over decades as hundreds of modules and local customizations were added by different VA medical centers.
What began as a streamlined platform eventually became a patchwork of site-specific versions that were costly to maintain, hard to upgrade, and nearly impossible to standardize. This uncontrolled feature creep turned a once-successful system into a fragmented liability—paving the way for today’s multi-billion-dollar modernization effort.
Once you start building, stakeholders inevitably request additional features that seem reasonable individually but collectively destroy budgets and timelines. Commercial EMRs force disciplined scope management through established feature sets.
Real-World EMR Disasters: Failures and Lessons Learned
Recent high-profile failures provide sobering lessons about custom EMR risks that every healthcare executive should understand.
Why Even Intermountain Healthcare Abandoned Their Homegrown System
Intermountain Healthcare's decision to abate its famous 40-year-old HELP system provides crucial insights. Despite investing $12 million for Meaningful Use certification in 2012, they found keeping the system modern would require continuous investment and ultimately switched to commercial Cerner.
Even with decades of successful operation, the regulatory environment made their sophisticated homegrown EMR unsustainable. Annual upkeep costs for legacy systems among six major health systems ranged from $21,000 to $1 million just in server costs, not including staff salaries.
VA's $50 Billion Modernization Nightmare
For decades, the VA ran VistA, a homegrown EMR widely praised by clinicians. But by the 2010s, it had become fragmented and outdated—unable to keep pace with interoperability, security, and modern data-sharing standards. What was once a success story had turned into a liability.
To replace it, the VA launched a commercial modernization project initially estimated at $10 billion. Costs have since ballooned toward $50 billion, while by 2023, only a handful of the VA’s 170+ medical centers had gone live.
With deployments paused after patient safety incidents, the VA’s experience shows how even the best homegrown EMR eventually collapses under its technical debt, forcing a far costlier and riskier replacement than starting with a commercial system from the outset.
Why Smart CTOs Say No: Risk Analysis Framework
Experienced healthcare technology leaders understand the career-limiting risks of custom EMR development. The fundamental question isn't whether you have IT staff - it's whether you have software engineers building products. If you don't have experienced software product developers, avoid custom EMR projects entirely.
Many clinic chains have traditional IT teams, but that's no substitute for real software developers building and maintaining products. Large health systems employ hundreds of Epic engineers, but much of their work is configuration, not true product engineering. There's a massive difference between configuring existing systems and building products from scratch.
The Maintenance Nightmare of Custom EMR
Once your custom EMR goes live, you effectively become a software company responsible for indefinite maintenance, support, and enhancements. This requires highly skilled developers, informaticists, and support personnel competing with tech companies for talent.
Intermountain reported spending $1.6 million annually on infrastructure and dedicated staff just to keep their old HELP system running in read-only mode for historical data access. This represents pure sunk cost, providing minimal new value.
PE Exit Implications: How Custom EMR Hurts Enterprise Value
Private equity buyers view custom EMRs as liabilities, not assets. They represent ongoing technical debt, vendor lock-in with your development team, and unknown risks. Acquirers prefer roll-ups onto existing standardized platforms rather than unique IP from clinic-built EMRs.
Commercial EMR implementations with proven track records are far more attractive to acquirers. Cost analysis, maintenance burden, and acquisition scenarios all make custom EMRs value-destructive investments.
The Strategic Alternative
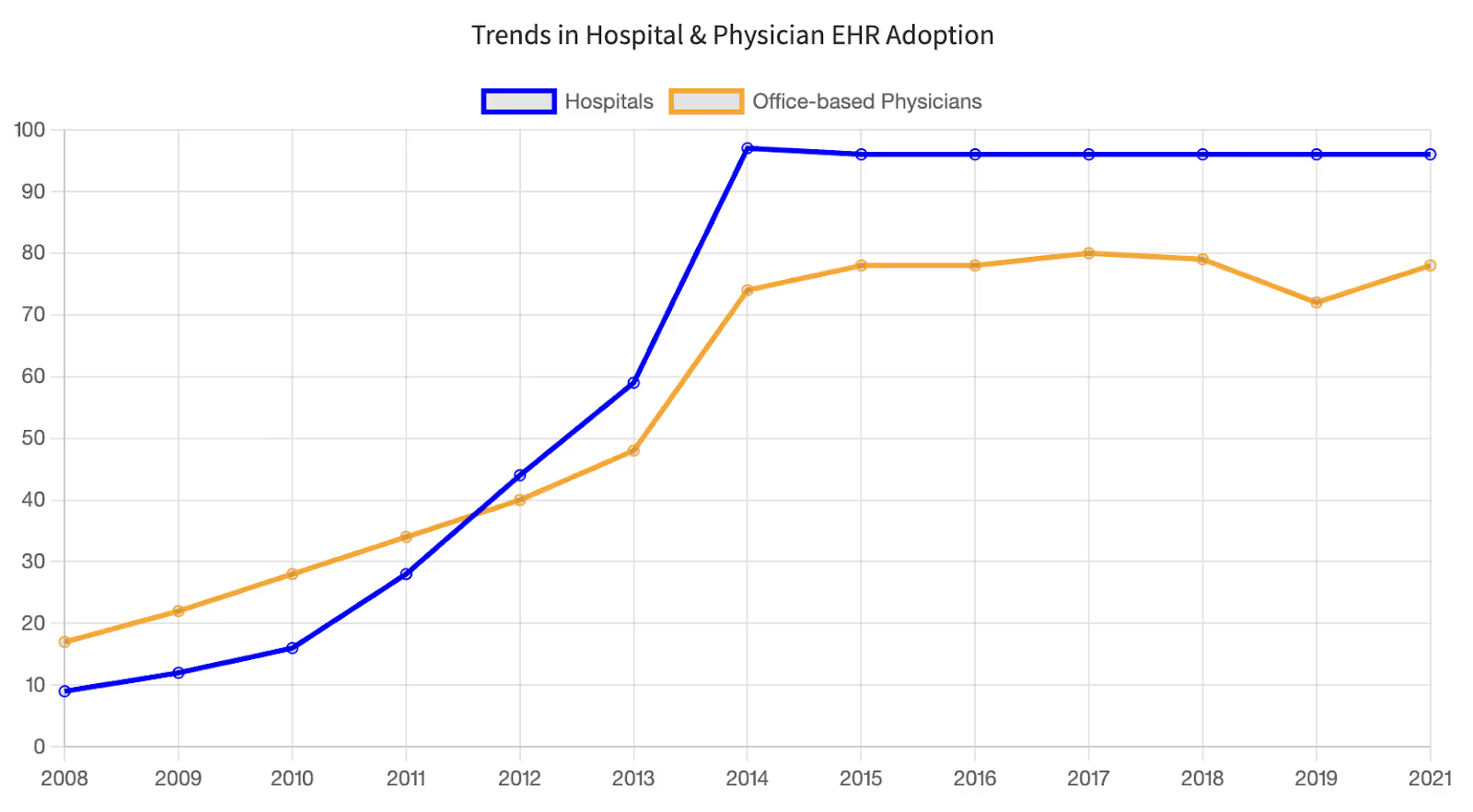
Instead of rebuilding the entire EMR wheel, smart organizations follow a simple principle: build around the EMR, don't build the EMR. As of 2021, 96% of U.S. hospitals and 78% of office-based physicians use certified EHR systems rather than homegrown ones.
The 95/5 Rule for Healthcare Technology
Roughly 95% of EMR functionality is commodity infrastructure: charting, scheduling, billing, labs, and prescriptions. Rebuilding these doesn't create a competitive advantage; it just burns capital. Focus your custom development resources on the 5% that truly differentiates your care model.
If your EMR creates workflow problems, automate around it using RPA. If it really sucks, switch vendors, but migration will take at least a year. Don't let EMR frustrations drive you toward custom development that wastes resources on commodity features.
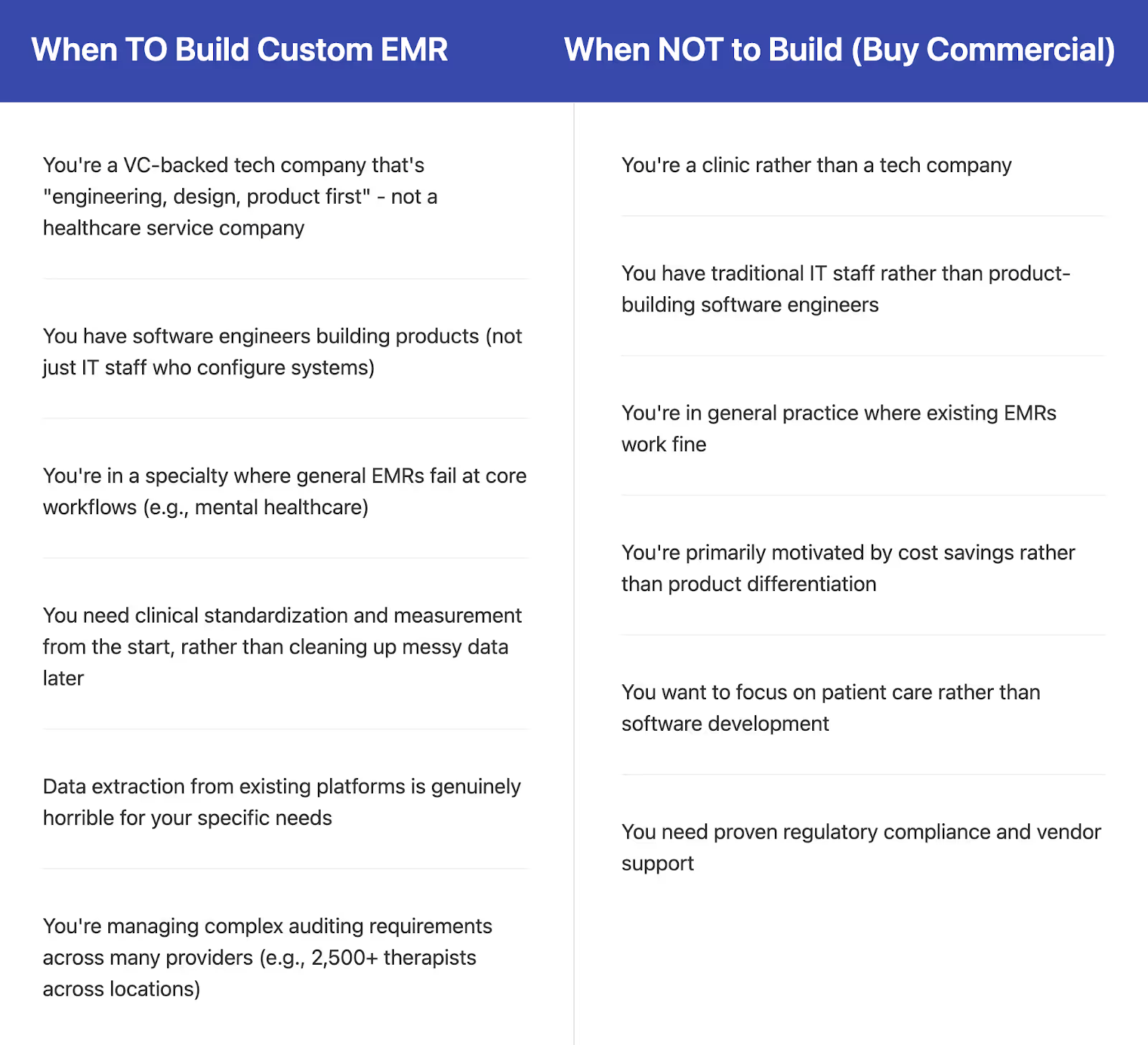
Build vs Buy Decision Framework
Consider hybrid approaches like Medplum, which provides an FHIR-compliant foundation while allowing custom frontend development. This works particularly well for tech-first startups building MVPs without starting from scratch.
For specialty-specific needs like mental healthcare workflows, focus on EMR customization or specialty modules rather than full custom development. Mental healthcare organizations often struggle because existing EMRs aren't designed for nuanced clinical workflows like assessments and psychological markers, lacking proper clinical measurement tools and standardized data capture for mental health workflows.
The data extraction problem compounds this issue - organizations managing 2,500+ providers across multiple locations who need to audit against payers find that existing platforms make this incredibly difficult. However, even a bare bones mental healthcare EMR isn't highly complex with modern backends and can often be addressed through integration platforms rather than full custom development.
What Actually Increases Enterprise Value
PE-backed healthcare organizations should focus on technology investments that demonstrably increase valuation multiples rather than create technical debt.
Technology Investments That Boost Valuation Multiples
Instead of custom EMR development, invest in revenue cycle automation that reduces days in AR, patient engagement platforms that increase retention, analytics overlays that optimize resource utilization, and API-first integrations that improve operational efficiency.
These targeted investments deliver measurable ROI while leveraging proven commercial platforms as the foundation.
Implementation Roadmap: Quick Wins While Avoiding the EMR Trap
Start with 90-day workflow optimization using your existing EMR's customization capabilities. Implement API-first integration strategies connecting your commercial EMR to specialty-specific tools. Negotiate better commercial terms before considering alternatives.
This delivers immediate improvements while preserving technical resources for truly differentiating capabilities.
Final Takeaways
Custom EMR development appears attractive when frustrated with commercial solutions, but the risks are devastating. Most projects face multi-year delays, budgets that balloon far beyond projections, and ongoing maintenance costs that consume 15–20% of the original build every year. Even well-resourced organizations routinely underestimate the complexity and long-term burden.
The fundamental issue is focus. Healthcare organizations aren't product companies. They consistently underestimate software complexity while underbudgeting for maintenance, all while being distracted from their core mission of excellent patient care.
The smart strategy focuses on the 5% of functionality that truly differentiates your organization. Build around the EMR, don't build the EMR. This approach delivers faster results, lower risk, and better long-term value creation without the nightmare of project failure.
Frequently Asked Questions
What's the biggest hidden cost in custom EMR development?
Regulatory compliance represents the largest hidden cost, consuming $500,000-1 million annually. Intermountain Healthcare spent $12 million just for Meaningful Use certification, yet still abandoned their custom system. Commercial vendors spread these costs across thousands of customers.
How do I know if my organization should never attempt custom EMR development?
If you have traditional IT staff rather than experienced software product developers, lack $15+ million in dedicated EMR budget, or can't commit 3-5 years to development, avoid custom EMR projects.
What should we do instead of building a custom EMR?
Adopt a leading commercial EHR and configure it extensively, consider specialty-specific EMR vendors, or implement modular solutions using FHIR APIs. Focus custom development on the 5% that differentiates your practice while leveraging proven platforms for commodity functionality.
How long do custom EMR projects actually take?
Most custom EMR projects require 3-5 years to reach basic functionality, if they succeed at all. The Coast Guard's project ran for five years before cancellation. Commercial implementations typically complete within 18-24 months across multi-hospital systems.
Don’t custom EMRs give us more control and flexibility?
Yes, but that control often leads to feature creep. Stakeholders keep requesting “just one more feature,” driving costs and delays. Commercial EMRs offer structured add-ons and governance processes that prevent this spiral.
What is the best alternative to custom EMR development?
The most effective strategy is to use a commercial EMR as your foundation and then extend it with custom modules, APIs, or integrations. This allows organizations to get the stability and scalability of a vendor system while tailoring the small percentage of functionality that sets them apart.
James founded Invene with a 20-year plan to build the world's leasing partner for healthcare innovation. A Forbes Next 1000 honoree, James specializes in helping mid-market and enterprise healthcare companies build AI-driven solutions with measurable PnL impact. Under his leadership, Invene has worked with 20 of the Fortune 100, achieved 22 FDA clearances, and launched over 400 products for their clients. James is known for driving results at the intersection of technology, healthcare, and business.
Ready to Tackle Your Hardest Data and Product Challenges?
We can accelerate your goals and drive measurable results.

